-
Author
Precious Moman -
PI
Dr. Peyman Benharash and Dr. Joshua Cohen
-
Co-Author
Mardock A, Mandelbaum A, Lai T, Zakhour M, Salani R
-
Title
Outcomes and Resource Utilization Following Surgery for Gynecologic Malignancies at Safety-Net Hospitals Across the United States
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
Outcomes and Resource Utilization Following Surgery for Gynecologic Malignancies at Safety-Net Hospitals Across the United States
Moman P, Mardock A, Mandelbaum A, Lai T, Zakhour M, Salani R, Benharash P, and Cohen JG
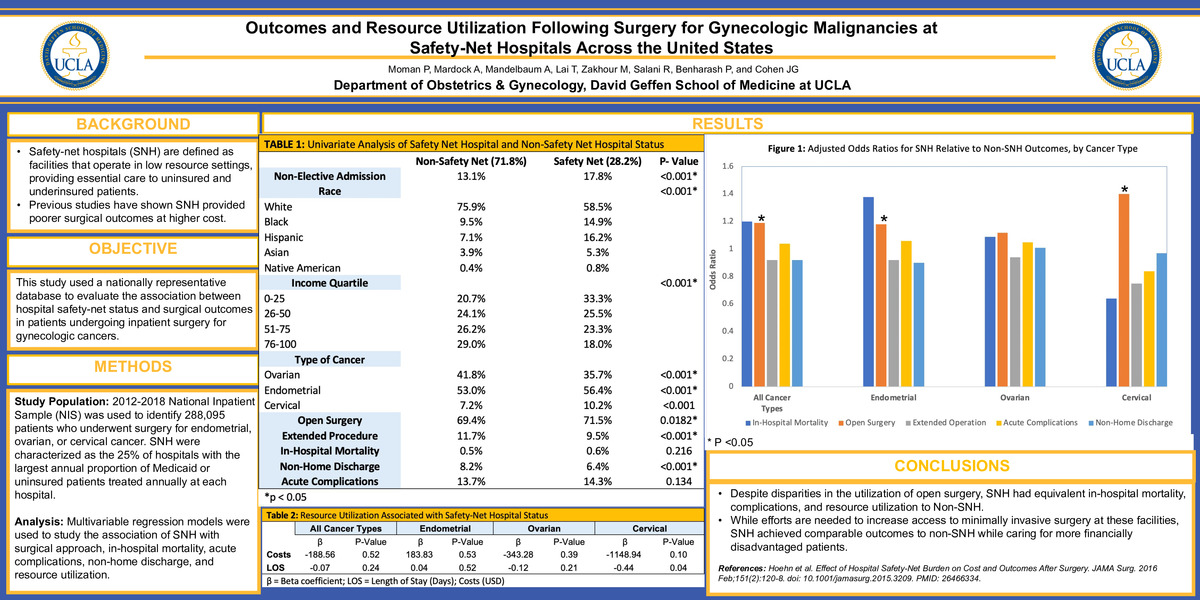
Objectives: To evaluate the association between hospital safety-net status and surgical outcomes among a national sample of patients undergoing inpatient surgery for gynecologic cancers. We hypothesized safety-net hospitals (SNH) to be associated with increased utilization of open surgery, in-hospital mortality, and acute complications.
Methods: The 2012-2018 National Inpatient Sample was used to identify all patients who underwent surgery for endometrial, ovarian, or cervical cancer. SNH were characterized as the 25% of hospitals with the largest annual proportion of Medicaid or uninsured patients treated annually at each hospital. Multivariable regression models were used to study the association of SNH with surgical approach, in-hospital mortality, acute complications, non-home discharge, and resource utilization.
Results: Of an estimated 288,015 patients, 28.2% were treated at SNH. Compared to non-SNH, an increased proportion of those treated at SNH were admitted non-electively (17.8% vs 13.1%, P<0.001), were identified as non-White race (41.5% vs 24.1%, P<0.001), and were in the lowest income quartile (33.3% vs 20.7%, P<0.001). SNH had a higher proportion of patients with endometrial (56.4% vs 53.0%, P<0.001) and cervical cancer (10.2% vs 7.2%, P<0.001), but relatively fewer patients with ovarian cancer (35.7% vs 41.8%, P<0.001). Compared to non-SNH, SNH had increased unadjusted rates of open surgery (71.5% vs 69.4%, P<0.001), but decreased rates of extended operations (9.5% vs 11.7%, P<0.001) and non-home discharge (6.4% vs 8.2%, P<0.001). Patients treated at SNH had similar unadjusted rates of in-hospital mortality (0.6% vs 0.5%, P=0.22) and acute complications (14.3% vs 13.7%, P=0.13). After adjustment for relevant variables including hospital surgical volume, SNH and non-SNH demonstrated equal likelihood of extended operation, mortality, complications, and non-home discharge for all cancer types (Table). Nevertheless, SNH remained associated with increased likelihood of open surgery compared to non-SNH for endometrial and cervical cancer patients. No significant association was observed between SNH and hospital cost or length of stay.
Conclusions: Despite disparities in the utilization of open surgery, SNH had equivalent in-hospital mortality, complications, and resource utilization. While efforts are needed to increase access to minimally invasive surgery at these facilities, SNH achieved comparable outcomes to non-SNH while caring for more financially disadvantaged patients.
Learning Objective: Learners will be able to demonstrate that safety-net hospitals achieved equivalent clinical outcomes and resource utilization to non-safety-net institutions following inpatient surgery for gynecologic cancers.
All Cancer Types
Endometrial
Ovarian
Cervical
AOR or β
P-Value
AOR or β
P-Value
AOR or β
P-Value
AOR or β
P-Value
In-Hospital Mortality
1.20
0.21
1.38
0.17
1.09
0.64
0.64
0.61
Open Surgery
1.19
<0.001
1.18
<0.001
1.12
0.08
1.40
<0.001
Extended Operation
0.92
0.07
0.92
0.31
0.94
0.20
0.75
0.12
Acute Complications
1.04
0.22
1.06
0.17
1.05
0.29
0.84
0.17
Non-Home Discharge
0.92
0.13
0.90
0.14
1.01
0.94
0.97
0.89
Costs ($)
-188.56
0.52
183.83
0.53
-343.28
0.39
-1148.94
0.10
Length of Stay (Days)
-0.07
0.24
0.04
0.52
-0.12
0.21
-0.44
0.04
-
PDF
-
Zoom
https://uclahs.zoom.us/j/96507150330?pwd=TWptQVUzTGtkaEkvMjl0Z3hiQ0VvUT09