-
Author
Jeremy Policht -
PI
Arya N. Shamie, M.D.
-
Co-Author
Alexander Upfill-Brown, M.D.
-
Title
National Trends in Lumbar Total Disc Replacement Utilization in the Treatment of Lumbar Degenerative Disc Disease from 2010- 2017
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
Abstract: National Trends in Lumbar Total Disc Replacement Utilization in the Treatment of Lumbar Degenerative Disc Disease from 2010- 2017
Study Design: Retrospective database study.
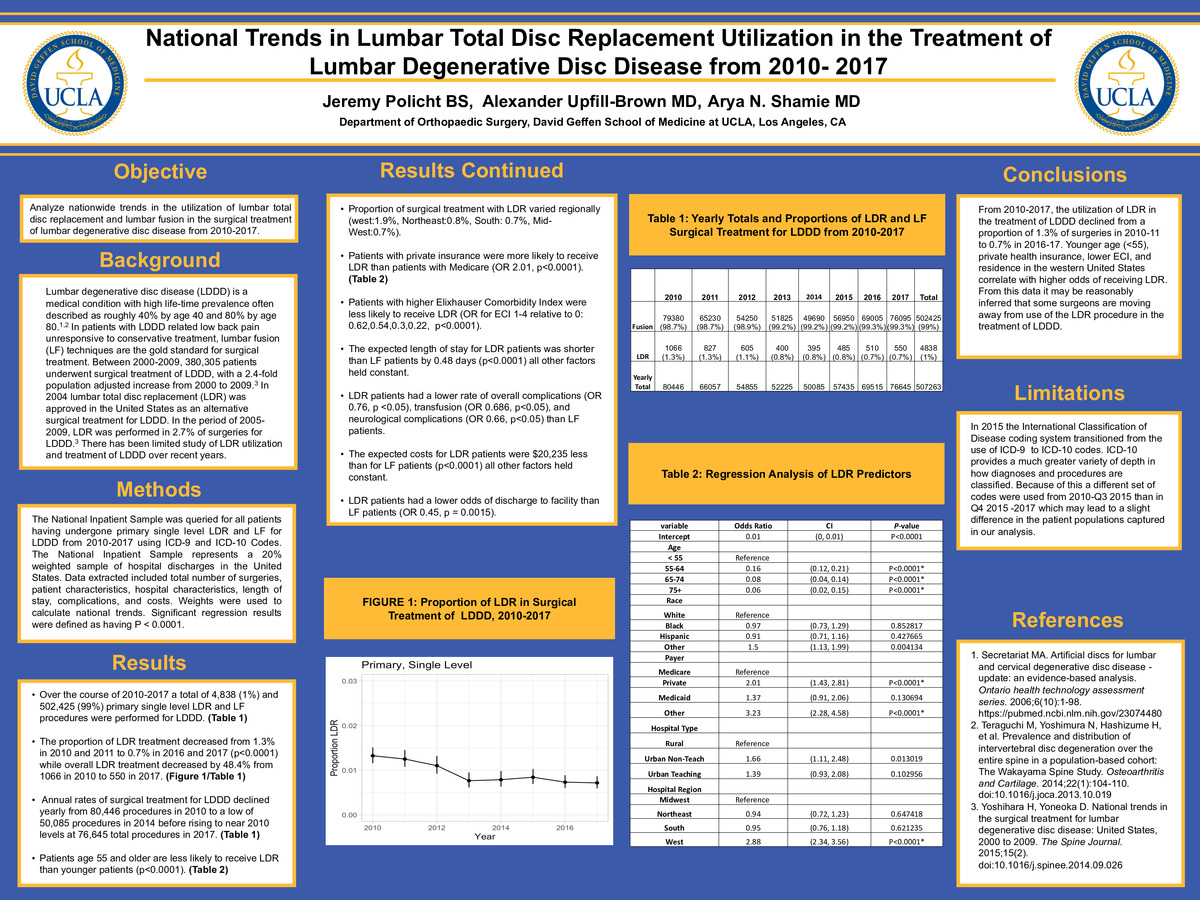
Objective: Analyze nationwide trends in the utilization of lumbar total disc replacement and lumbar fusion in the surgical treatment of lumbar degenerative disc disease from 2010-2017.
Background: Lumbar degenerative disc disease (LDDD) is a medical condition with high lifetime prevalence often described as roughly 40% by age 40 and 80% by age 80. In patients with LDDD related low back pain unresponsive to conservative treatment, lumbar fusion (LF) techniques are the gold standard for surgical treatment. Between 2000-2009, 380,305 patients underwent surgical treatment of LDDD, with a 2.4-fold population-adjusted increase from 2000 to 2009. In 2004 lumbar total disc replacement (LDR) was approved in the United States as an alternative surgical treatment for LDDD. In the period of 2005-2009, LDR was performed in 2.7% of surgeries for LDDD. There has been limited study of LDR utilization and treatment of LDDD over recent years.
Methods: The National Inpatient Sample was queried for all patients having undergone primary single level LDR and LF for LDDD from 2010-2017 using ICD-9 and ICD-10 Codes. The National Inpatient Sample represents a 20% weighted sample of hospital discharges in the United States. Data extracted included the total number of surgeries, patient characteristics, hospital characteristics, length of stay, complications, and costs. Weights were used to calculate national trends. Significant regression results were defined as having P < 0.0001.
Results: Over the course of 2010-2017 a total of 4,838 (1%) and 502,425 (99%) primary single level LDR and LF procedures were performed for LDDD. The proportion of LDR treatment decreased from 1.3% in 2010 and 2011 to 0.7% in 2016 and 2017 (p<0.0001) while overall LDR treatment decreased by 48.4% from 1066 in 2010 to 550 in 2017. Annual rates of surgical treatment for LDDD declined yearly from 80,446 procedures in 2010 to a low of 50,085 procedures in 2014 before rising to near 2010 levels at 76,645 total procedures in 2017. Patients age 55 and older were less likely to receive LDR than younger patients (p<0.0001). Over this timespan, 2% of patients treated for LDDD age < 55 underwent lumbar total disc replacement compared to less than 0.15% for older patients. Proportion of surgical treatment with LDR varied regionally (west:1.9%, Northeast:0.8%, South: 0.7%, Mid-West:0.7%). Patients with private insurance were more likely to receive LDR than patients with Medicare (OR 2.01, p<0.0001). Patients with a higher Elixhauser Comorbidity Index were less likely to receive LDR (OR for ECI 1-4 relative to 0: 0.62,0.54,0.3,0.22, p<0.0001). The expected length of stay for LDR patients was shorter than LF patients by 0.48 days (p<0.0001) all other factors held constant. The expected costs for LDR patients were $20,235 less than for LF patients (p<0.0001) all other factors held constant.
LDR patients had a lower rate of overall complications (OR 0.76, p <0.05), transfusion (OR 0.686, p<0.05), and neurological complications (OR 0.66, p<0.05) than LF patients. LDR patients had a lower odds of discharge to facility than LF patients (OR 0.45, p = 0.0015).
Conclusions: From 2010-2017, the utilization of LDR in the treatment of LDDD declined from a proportion of 1.3% of surgeries in 2010-11 to 0.7% in 2016-17. Younger age (<55), private health insurance, lower ECI, and residence in the western United States correlate with higher odds of receiving LDR. From this data, it may be reasonably inferred that some surgeons are moving away from the use of the LDR procedure in the treatment of LDDD.
Limitations: In 2015 the International Classification of Disease coding system transitioned from the use of ICD-9 to ICD-10 codes. ICD-10 provides a much greater variety of depth in how diagnoses and procedures are classified. Because of this, a different set of codes was used from 2010-Q3 2015 than in Q4 2015 -2017 which may lead to a slight difference in the patient populations captured in our analysis.
References:
1. Secretariat MA. Artificial discs for lumbar and cervical degenerative disc disease -update: an evidence-based analysis. Ontario health technology assessment series. 2006;6(10):1-98. https://pubmed.ncbi.nlm.nih.gov/23074480
2. Teraguchi M, Yoshimura N, Hashizume H, et al. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: The Wakayama Spine Study. Osteoarthritis and Cartilage. 2014;22(1):104-110. doi:10.1016/j.joca.2013.10.019
3. Yoshihara H, Yoneoka D. National trends in the surgical treatment for lumbar degenerative disc disease: United States, 2000 to 2009. The Spine Journal. 2015;15(2). doi:10.1016/j.spinee.2014.09.026
-
PDF
-
Zoom