-
Author
Doorga Ghosh -
PI
Dr. Elizabeth L. Lord
-
Co-Author
-
Title
Prevalence and Impact of Cannabinoid Use in Patients with Spinal Disorders
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
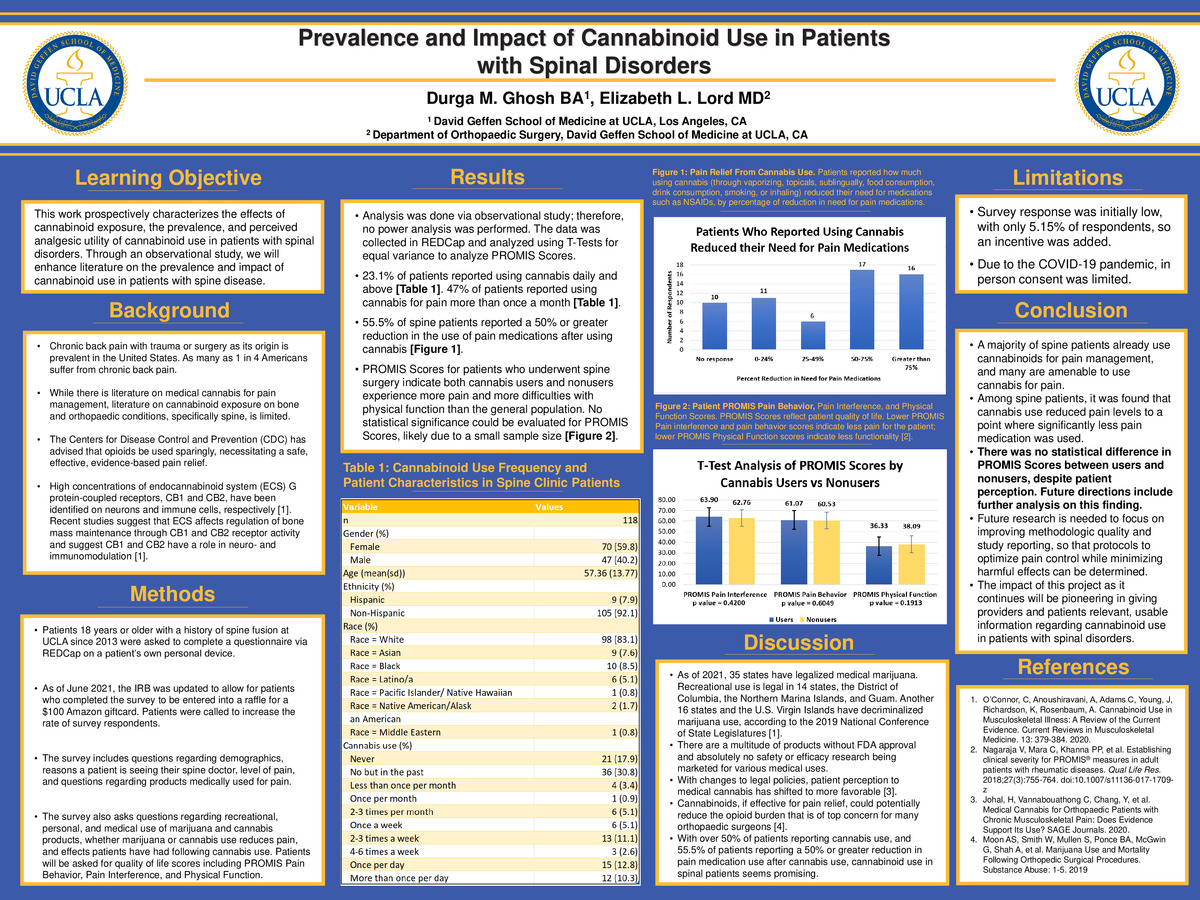
ABSTRACT: This study will explore the prevalence and perceived analgesic utility of cannabinoid use in patients with spinal disorders. Chronic back pain with trauma or surgery as its origin is prevalent in the United States, with as many as 1 in 4 Americans suffering from chronic back pain. The Centers for Disease Control and Prevention (CDC) has advised that opioids be used sparingly, necessitating a safe, effective, evidence-based pain relief. Cannabinoids are becoming increasingly legal, accepted, and used in the United States and worldwide, however there are a multitude of products without FDA approval and absolutely no safety or efficacy research, being marketed for various medical uses. Cannabis is also becoming increasingly popular in medical settings. As of 2021, 35 states have legalized medical marijuana, with recreational use legal in 14 states, the District of Columbia, the Northern Marina Islands, and Guam. Another 16 states and the U.S. Virgin Islands have decriminalized the use of marijuana at the time of writing, according to the 2019 National Conference of State Legislatures [1]. Through an observational study, we plan to enhance literature on the prevalence and impact of cannabinoid use in patients with spine disease. We hypothesize that there will be a difference in pain perception, opioid consumption, and quality of life in cannabis users.
PURPOSE: The proposed study will prospectively characterize, for the first time, the effects of cannabinoid exposure in patients with musculoskeletal (MSK) disorders.
BACKGROUND: While there is a large body of literature on medical cannabis for pain management, the literature related to cannabinoid exposure on bone and orthopaedic conditions is limited. Musculoskeletal pain is a “clear driver” of the opioid epidemic, with acute and chronic musculoskeletal pain management being cited as a leading reason patients seek opioid prescriptions [2]. Chronic pain is quite prevalent and can be debilitating, as well as cause socioeconomic burdens. There is a clear need for more efficacious therapies.
Self-reported use of cannabinoids has increased following the legalization of recreational and medical use. Over 22 million Americans over the age of 12 used marijuana in 2016 [3]. Among orthopaedic patients, a decreased inpatient mortality rate has been noted in patients who used marijuana, compared to non-users [3].
High concentrations of endocannabinoid system (ECS) G protein-coupled receptors, CB1 and CB2, have been identified on neurons and immune cells, respectively [4]. Recent studies suggest that ECS affects regulation of bone mass maintenance through CB1 and CB2 receptor activity and suggest CB1 and CB2 have a role in neuro- and immunomodulation [4]. CB1 receptor activity also specifically appears to have a protective role in regulating bone mass and osteoporosis through adipocyte and osteoblast differentiation [2]. Pre-clinical studies demonstrate that cannabinoid signaling has an integral role in the nociceptive system and that CB1 and CB2 receptor agonists have antinociceptive properties [4]. This indicates that CBD may increase bone healing through activating cannabinoid receptors, and THC likely inhibits bone metabolism [4]. Alternatives to narcotic use have gained substantial attention and the efficacy of cannabinoid use could encourage cannabinoid use for musculoskeletal pain management.
Among the chemical constituents of cannabis, THC is the most considerably studied, and is responsible for most of the physical and psychotropic effects [5]. CBD, the second most prevalent cannabinoid in most cannabis strains, has counter effects to that of THC – less psychoactive potential and more calming and anti-inflammatory effects [5]. However, there is large variation in the route of administration and dosage relating to cannabis, causing variability with interactions with the body’s ECS. There is also considerable variation in CB1 and CB2 receptor expression. CB1 receptors are highly localized to the central and peripheral nervous system whereas CB2 receptor expression is greatest in the immune tissues and can be found in bone and muscle [4].
In mice models, central and peripheral endocannabinoids have been shown to contribute to spinal manipulative therapy analgesia [6]. The endocannabinoid system has been proposed to play a role in decreased inflammatory cascade, enhancing pain management [7]. While there is data on the potential benefits of cannabinoid use, no one study has determined efficacy in the patient population we are studying. Retrospective studies have also been conducted, such as a study examining the impact of cannabis use on total keen arthroplasty (TKA) revision incidence, revision causes, and time to revision. Through analyzing the Medicare database between 2005 and 2014, it was determined that cannabis use “may” result in decreasing implant survivorship and increasing risk for revision compared to non-cannabis users following primary TKA [8]. However, evidence on cannabinoids in the musculoskeletal patients based on high-quality clinical trials are limited [2].
Current evidence suggests medical cannabis use is effective for some types of pain, however, this efficacy was demonstrated only when there was either no comparator or cannabis was compared with a placebo [9]. Low-to-moderate quality evidence shows that cannabinoids are associated with a “small, but statistically significant” reduction in chronic pain scores, compared with placebo [2]. Results from systematic reviews have demonstrated more adverse events in cannabinoid groups than in placebo groups with longer than 2 weeks of treatment, but there is a lack of evidence on dependence [2].
With changes to legal policies, patient perception has changed to shift towards more favorably viewing the use of medical cannabis [2]. Cannabinoids, if effective for pain relief, could potentially reduce the opioid burden that is of top concern for many orthopaedic surgeons [3]. While pre-clinical studies demonstrate the important role ECS has in bone healing homeostasis, it is not clear whether this will correlate with clinical trials.
METHODS: For this study, patients 18 years or older with a history of spine fusion at UCLA since 2013 will be asked to complete a questionnaire. The survey will be administered via REDCap survey on patient’s own personal devices. The survey will be offered to each patient, new or returning, only once across all clinics. Patients will be notified they should only complete the survey once. There is a unique study ID generated at the recruitment stage, which is linked to the survey. The surveys do not contain PHI.
As of June 2021, the IRB was updated to allow for patients who completed the survey to be entered into a raffle for a $100 Amazon giftcard. Patients were called to increase the rate of survey respondents.
The survey includes questions regarding demographics, reasons a patient is seeing their spine doctor, level of pain, and questions regarding products medically used for pain. The survey also asks questions regarding recreational, personal, and medical use of marijuana and cannabis products, whether marijuana or cannabis use reduces pain, and effects patients have had following cannabis use. They will also be asked for quality of life scores including PROMIS Pain Behavior, Pain Interference, and Physical Function.
PRELIMINARY RESULTS: Analysis was done via observational study; therefore no power analysis was performed. The data was collected in REDCap and analyzed using T-Tests for equal variance to analyze PROMIS Scores and test for any significant differences between the means calculated for cannabis users and nonusers.
23.1% of patients reported using cannabis daily and above for pain [Table 1]. 47% of patients reported using cannabis for pain more than once a month [Table 1]. 55.5% of spine patients reported a 50% or greater reduction in the use of pain medications after using cannabis for pain [Figure 1].
PROMIS scores for patients who underwent spine surgery indicate both cannabis users and nonusers experience more pain and more difficulties with physical function than the general population. For both spine patient groups, cannabis users and nonusers, PROMIS Pain Interference and PROMIS Pain Behavior Scores were greater than 60. A score of 60 is one standard deviation from the mean, indicating spine patients experience greater levels of pain after surgery, which was to be expected. A lower PROMIS Physical Function score indicates a greater difficulty in physical tasks for patients. No statistical significance could be evaluated for PROMIS Scores between cannabis users and nonusers, likely due to a small sample size [Figure 2].
CONCLUSIONS: A majority of spine patients already use cannabinoids for pain management, and many are amenable to use cannabis for pain. Among spine patients, it was discovered through this study that cannabis use reduced pain levels to a point where significantly less pain medication was used. There was no statistical difference in PROMIS Scores between users and nonusers, despite patient perception. Future directions include further analysis on this finding. Additionally, future research is needed to focus on improving methodologic quality and study reporting, so that protocols to optimize pain control while minimizing harmful effects can be determined. The impact of this project as it continues will be pioneering in giving providers and patients relevant, usable information regarding use of cannabinoids in patients with spinal disorders.
FUTURE DIRECTIONS: This project is ongoing. It was particularly interesting to discover that the P values for PROMIS Scores between users and nonusers was not stastically significant, so further research will delve into this nuance. Next steps also include continuing to consent patients to increase our sample size. Future directions can also include further analysis on demographics, methods of cannabis use, and dosage as well as strain of cannabis.
REFERENCES:
- National Conference of State Legislatures. Marijuana Overview. October 17, 2019.
- Johal, H, Vannabouathong C, Chang, Y, et al. Medical Cannabis for Orthopaedic Patients with Chronic Musculoskeletal Pain: Does Evidence Support Its Use? SAGE Journals. 2020.
- Moon AS, Smith W, Mullen S, Ponce BA, McGwin G, Shah A, et al. Marijuana Use and Mortality Following Orthopedic Surgical Procedures. Substance Abuse: 1-5. 2019
- O’Connor, C, Anoushiravani, A, Adams C, Young, J, Richardson, K, Rosenbaum, A. Cannabinoid Use in Musculoskeletal Illness: A Review of the Current Evidence. Current Reviews in Musculoskeletal Medicine. 13: 379-384. 2020.
- Ashton, CH. Pharmacology and Effects of Cannabis: A Brief Review. Br J Psychiatry. 178: 101–106. 2001.
- Fitzcharles, M, Hauser W. Cannabinoids in the Management of Musculoskeletal or Rheumatic Diseases. Current Rheumatology Reports. 2016.
- Kleeman-Forshuber, L, Dennis, D, Jennings J. Medicinal Cannabis in Orthopaedic Practice. Journal of the American Academy of Orthopaedic Surgery. 2020.
- Law, TY, et al. Cannabis Use Increases Risk for Revision After Total Knee Arthroplasty. Journal of Long-Term Effects of Medical Implants. 125-130. 2019.
- Madden, K et al. Cannabis for Pain in Orthopedics: A Systematic Review Focusing on Study Methodology. Canadian Journal of Surgery. 2019.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/99607615825?pwd=NE9oT2t2NHp0VVh4ai9Nb2ZYL3AvZz09