-
Author
Sahar Alimirzaie -
PI
Justine C. Lee, MD, PhD
-
Co-Author
Sarah Mirzaie, BS; Michelle Oberoi, BS; Rachel Caprini, BS; Kelly Huang; Harshini Malapati BS; Justine C. Lee, MD, PhD
-
Title
Self-Reported Anxiety Independently Predicts Increased Perioperative Opioid Usage in Pediatric Craniofacial Surgeries
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
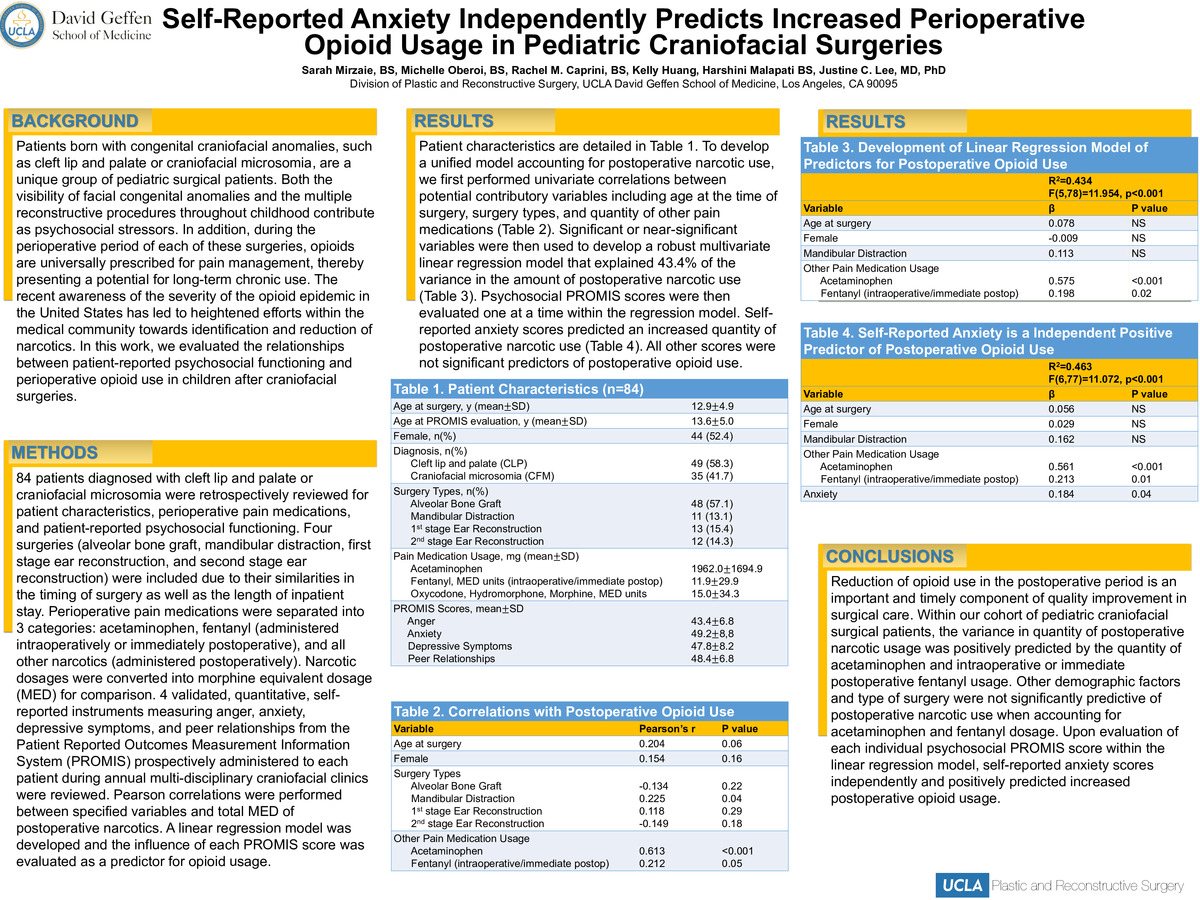
Introduction: Patients born with congenital craniofacial anomalies, such as cleft lip and palate or craniofacial microsomia, are a unique group of pediatric surgical patients. Both the visibility of facial congenital anomalies and the multiple reconstructive procedures throughout childhood contribute as psychosocial stressors. In addition, during the perioperative period of each of these surgeries, opioids are universally prescribed for pain management, thereby presenting a potential for long-term chronic use. The recent awareness of the severity of the opioid epidemic in the United States has led to heightened efforts within the medical community towards identification and reduction of narcotics. In this work, we evaluated the relationships between patient-reported psychosocial functioning and perioperative opioid use in children after craniofacial surgeries.
Methods: 84 patients diagnosed with cleft lip and palate or craniofacial microsomia were retrospectively reviewed for patient characteristics, perioperative pain medications, and patient-reported psychosocial functioning. Four surgeries (alveolar bone graft, mandibular distraction, first stage ear reconstruction, and second stage ear reconstruction) were included due to their similarities in the timing of surgery as well as the length of inpatient stay. Perioperative pain medications were separated into 3 categories: acetaminophen, fentanyl (administered intraoperatively or immediately postoperative), and all other narcotics (administered postoperatively). Narcotic dosages were converted into morphine equivalent dosage (MED) for comparison. 4 validated, quantitative, self-reported instruments measuring anger, anxiety, depressive symptoms, and peer relationships from the Patient Reported Outcomes Measurement Information System (PROMIS) prospectively administered to each patient during annual multi-disciplinary craniofacial clinics were reviewed. Pearson correlations were performed between specified variables and total MED of postoperative narcotics. A linear regression model was developed and the influence of each PROMIS score was evaluated as a predictor for opioid usage.
Results: Patient characteristics are detailed in Table 1. To develop a unified model accounting for postoperative narcotic use, we first performed univariate correlations between potential contributory variables including age at the time of surgery, surgery types, and quantity of other pain medications (Table 2). Significant or near-significant variables were then used to develop a robust multivariate linear regression model that explained 43.4% of the variance in the amount of postoperative narcotic use (Table 3). Psychosocial PROMIS scores were then evaluated one at a time within the regression model. Self-reported anxiety scores predicted an increased quantity of postoperative narcotic use (Table 4). All other scores were not significant predictors of postoperative opioid use.
Conclusions: Reduction of opioid use in the postoperative period is an important and timely component of quality improvement in surgical care. Within our cohort of pediatric craniofacial surgical patients, the variance in quantity of postoperative narcotic usage was positively predicted by the quantity of acetaminophen and intraoperative or immediate postoperative fentanyl usage. Other demographic factors and type of surgery were not significantly predictive of postoperative narcotic use when accounting for acetaminophen and fentanyl dosage. Upon evaluation of each individual psychosocial PROMIS score within the linear regression model, self-reported anxiety scores independently and positively predicted increased postoperative opioid usage.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/91060460857?pwd=YVcvTm5OejQ5bGVzeWFLZjMzZlFWUT09