-
Author
David Zarrin -
PI
Geoffrey Colby
-
Co-Author
David Zarrin
-
Title
Neuromodulation of the Autonomic Nervous System for Regulation of Cerebral Blood Flow
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
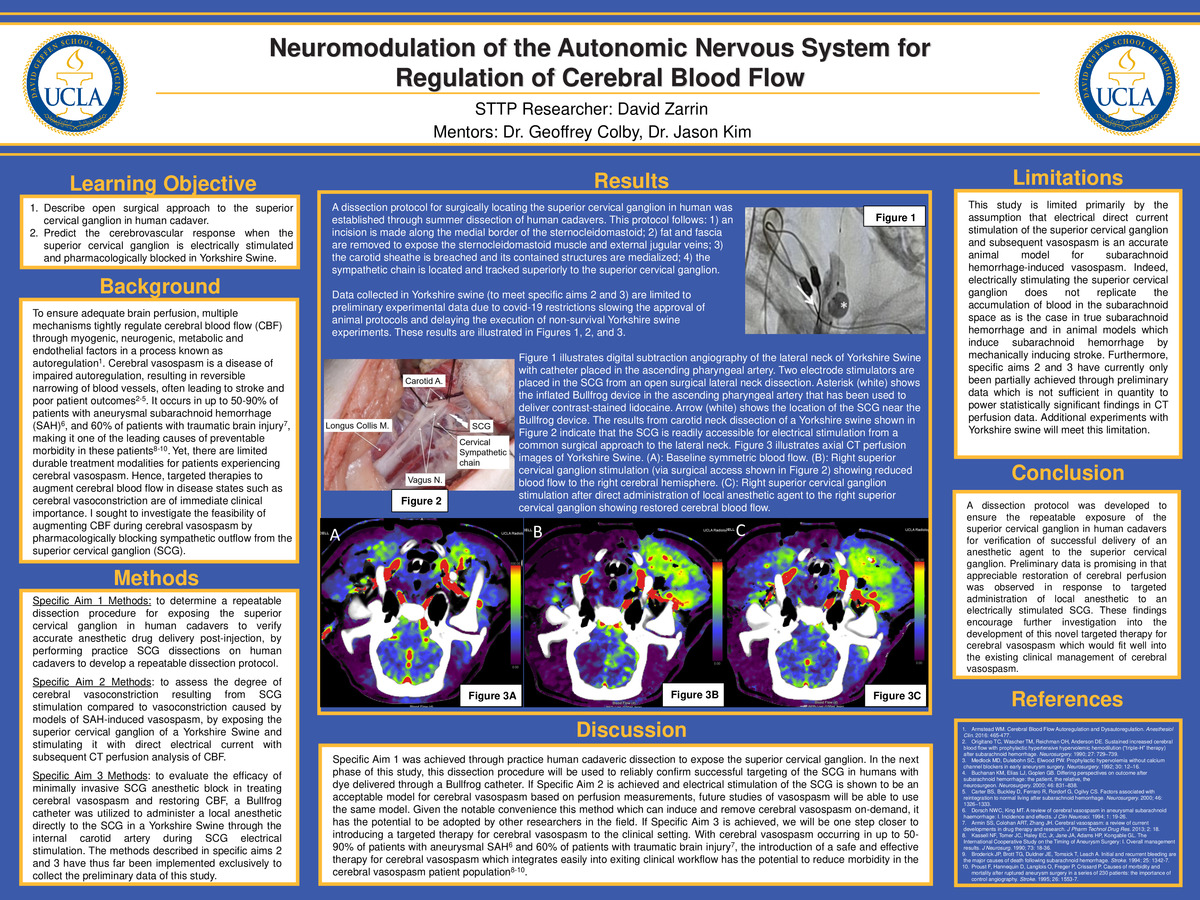
To ensure adequate brain perfusion, multiple mechanisms tightly regulate cerebral blood flow (CBF) through myogenic, neurogenic, metabolic and endothelial factors in a process known as autoregulation [1]. Cerebral vasospasm is a disease of impaired autoregulation, resulting in reversible narrowing of blood vessels, often leading to stroke and poor patient outcomes [2-5]. It occurs in up to 50-90% of patients with aneurysmal subarachnoid hemorrhage (SAH) [6], and 60% of patients with traumatic brain injury [7], making it one of the leading causes of preventable morbidity in these patients [8-10]. Yet, there are limited durable treatment modalities for patients experiencing cerebral vasospasm; intra-arterial calcium channel blockers are moderately effective but short-acting, and balloon angioplasty has limited access to distal vessels with higher risks of vessel dissection and rupture. Hence, targeted therapies to augment cerebral blood flow in disease states such as cerebral vasoconstriction are of immediate clinical importance. For my summer research project, I sought to investigate the feasibility of augmenting cerebral perfusion during cerebral vasospasm by pharmacologically blocking sympathetic outflow from the superior cervical ganglion.
[1] Armstead WM. Cerebral Blood Flow Autoregulation and Dysautoregulation. Anesthesiol Clin. 2016: 465-477.
[2] Origitano TC, Wascher TM, Reichman OH, Anderson DE. Sustained increased cerebral blood flow with prophylactic hypertensive hypervolemic hemodilution (“triple-H” therapy) after subarachnoid hemorrhage. Neurosurgery. 1990; 27: 729–739.
[3] Medlock MD, Dulebohn SC, Elwood PW. Prophylactic hypervolemia without calcium channel blockers in early aneurysm surgery. Neurosurgery. 1992; 30: 12–16.
[4] Buchanan KM, Elias LJ, Goplen GB. Differing perspectives on outcome after subarachnoid hemorrhage: the patient, the relative, the neurosurgeon. Neurosurgery. 2000; 46: 831–838.
[5] Carter BS, Buckley D, Ferraro R, Rordorf G, Ogilvy CS. Factors associated with reintegration to normal living after subarachnoid hemorrhage. Neurosurgery. 2000; 46: 1326–1333.
[6] Dorsch NWC, King MT. A review of cerebral vasospasm in aneurysmal subarachnoid haemorrhage: I. Incidence and effects. J Clin Neurosci. 1994; 1: 19-26.
[7] Armin SS, Colohan ART, Zhang JH. Cerebral vasospasm: a review of current developments in drug therapy and research. J Pharm Technol Drug Res. 2013; 2: 18.
[8] Kassell NF, Tomer JC, Haley EC, Jr, Jane JA, Adams HP, Kongable GL. The International Cooperative Study on the Timing of Aneurysm Surgery: I. Overall management results. J Neurosurg. 1990; 73: 18-36.
[9] Broderick JP, Brott TG, Duldner JE, Tomsick T, Leach A. Initial and recurrent bleeding are the major causes of death following subarachnoid hemorrhage. Stroke. 1994; 25: 1342-7.
[10] Proust F, Hannequin D, Langlois O, Freger P, Crissard P. Causes of morbidity and mortality after ruptured aneurysm surgery in a series of 230 patients: the importance of control angiography. Stroke. 1995; 26: 1553-7.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/97007672403?pwd=OWY3TjErckZQMXhTRCs4ejFFNFd3Zz09