-
Author
Chelsea Pan -
PI
Dr. Peyman Benharash
-
Co-Author
Chelsea Pan BA, Zachary Tran MD, Joseph Hadaya MD, Samuel Kim BA, Arjun Verma, Yas Sanaiha MD, Peyman Benharash MD
-
Title
Pericardiocentesis vs Surgical Drainage: A National Comparison of Clinical Outcomes and Resource Utilization
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
Purpose
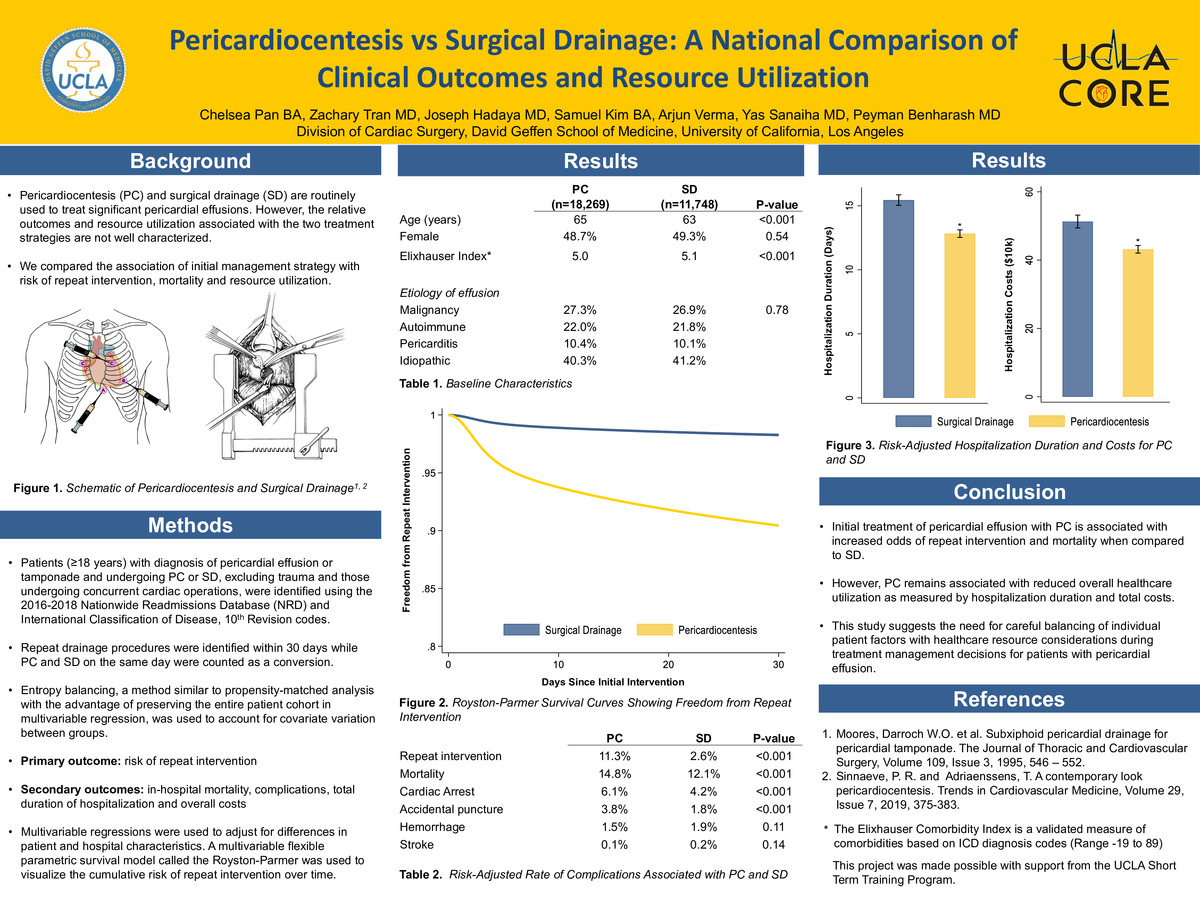
Pericardiocentesis (PC) or surgical drainage (SD) is routinely used to treat significant pericardial effusions. However, the relative outcomes and resource utilization associated with the two treatment strategies have not been well characterized at a national level. The present study aimed to compare the association of initial management strategy with risk of repeat intervention, mortality and resource utilization.
Methods
The 2016-2018 Nationwide Readmissions Database was queried to identify all patients (>=18 years) with a diagnosis of pericardial effusion or tamponade and undergoing PC or SD using International Classification of Disease 10th Revision codes. Those with traumatic injury or undergoing other cardiac operations were excluded. Patients were grouped by initial treatment strategy as PC or SD. Repeat drainage procedures were identified within 30 days while PC and SD on the same day were counted as a conversion. Entropy balancing, a method similar to propensity-matched analysis with the advantage of preserving the entire patient cohort in multivariable regression, was used to account for covariate variation between groups. The primary outcome of interest was difference in risk of reintervention between procedure type, while secondary endpoints included comparisons of in-hospital mortality, total duration of hospitalization and overall costs.
Results
Of an estimated 30,017 patients included for analysis, 18,269 (60.9%) were managed with PC. Compared to SD, PC patients were older (65 years vs 63, p<0.001) and had fewer comorbidities as defined by the Elixhauser Comorbidity Index (5.0 vs 5.1, p<0.001). Patients undergoing PC had higher unadjusted rates of mortality (11.1% vs 8.5, p<0.001) and reintervention within 30 days of initial operation (11.3% vs 2.7, p<0.001) which occurred predominantly on the index admission (76.5%). Primary reintervention strategy following PC was SD (84.5%). After adjustment with entropy balancing, PC patients remained at significantly increased risk for reintervention (11.3% vs 2.6, p<0.001) as well as mortality (14.8% vs 12.1, p<0.001) relative to SD. Despite increased odds of reintervention, PC was associated with a shorter duration of hospitalization (b: -2.6 days, 95% CI -3.1 to -2.1) and lower costs (b: -$8,000, 95% CI -$10,200 to -$5,800).
Conclusion
Initial treatment of pericardial effusion with PC is associated with increased odds of repeat intervention as well as mortality when compared to SD. However, PC remains associated with reduced overall healthcare utilization as measured by hospitalization duration and total costs. This study suggests the need for careful balancing of individual patient factors with healthcare resource considerations during treatment management decisions for patients with pericardial effusion.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/91601977470?pwd=dVhad0UybkNWTGhEaUtBYW5mL2pZUT09