-
Author
Fahim Mahmud -
PI
Dr. Howard C. Jen
-
Co-Author
-
Title
Racial Disparities in 30-Day Postoperative Outcomes of Risk-Stratified Congenital Diaphragmatic Hernia Repair
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
Background
Congenital malformations are the leading cause of infant mortality in the United States (21% of infant deaths). Among patients with birth defects, congenital diaphragmatic hernia (CDH) contributes the largest total number of in-hospital neonatal deaths in the United States. CDH occurs as a result of incomplete diaphragm formation during embryogenesis. Abdominal viscera herniate into the fetal chest cavity, and the resulting pulmonary hypoplasia and pulmonary hypertension can cause cardiorespiratory failure in the neonatal period.
Clinical Prediction Models (CPM’s) utilize clinical information (predictors) to estimate the probability of certain clinical outcomes and aid in clinical decision making. There have been a number of CPM's attempting to risk stratify CDH infants based on their pre- and postnatal presentation. In 2014, Brindle et al. and the Congenital Diaphragmatic Hernia Study Group (CDHSG) published an updated, simplified CPM to stratify CDH infants based on their disease severity within the first few hours of life and identify those at high risk for mortality.
Race has been shown to be a significant factor in CDH survival rates; however, there have been few studies incorporating race as a factor in CPMs. In this study, we aim to apply the CDHSG CPM to risk stratify a national sample of infants undergoing CDH repair and determine racial disparities in 30-day postoperative mortality and morbidity outcomes.
Methods
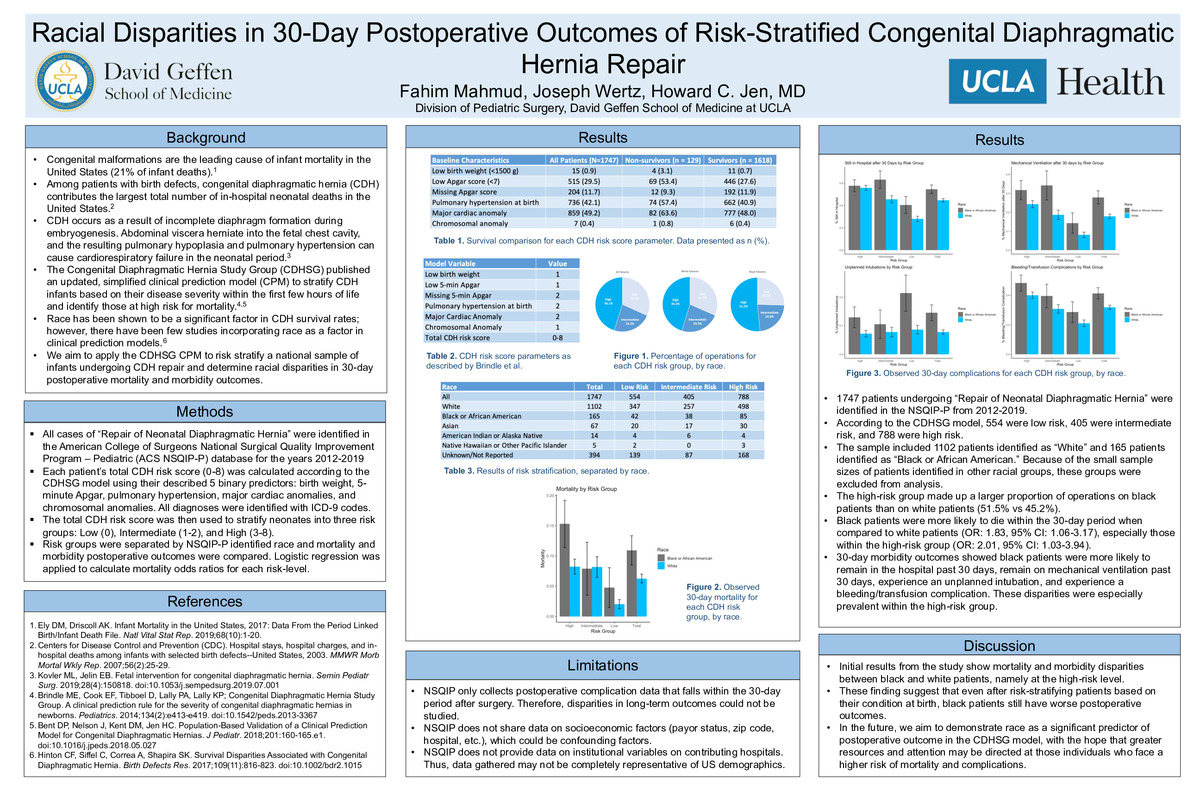
Using the American College of Surgeons National Surgical Quality Improvement Program – Pediatric (ACS NSQIP-P) database for the years 2012-2019, all procedures with the CPT code for “Repair of Neonatal Diaphragmatic Hernia” were identified. Each patient’s total CDH risk score (0-8) was calculated according to the CDHSG model using their described 5 binary predictors: birth weight, 5-minute Apgar, pulmonary hypertension, major cardiac anomalies, and chromosomal anomalies. All diagnoses were identified with ICD-9 codes. The total CDH risk score was then used to stratify neonates into three risk groups: Low (0), Intermediate (1-2), and High (3-8). Each risk group was separated by the NSQIP-P identified race. The NSQIP-P data guide was then used to identify 30-day postoperative outcome variables, including survival, length of hospital stay, length of mechanical ventilation, unplanned intubations, and bleeding/transfusion complications. Logistic regression was applied to calculate mortality odds ratios for each risk-level.
Results
1747 patients undergoing “Repair of Neonatal Diaphragmatic Hernia” were identified in the NSQIP-P from 2012-2019. According to the CDHSG model, 554 were low risk, 405 were intermediate risk, and 788 were high risk. The sample included 1102 patients identified as “White” and 165 patients identified as “Black or African American.” Because of the small sample sizes of patients identified in other racial groups, these groups were excluded from analysis. The high-risk group made up a larger proportion of operations on black patients than on white patients (51.5% vs 45.2%). Black patients were more likely to die within the 30-day period when compared to white patients (OR: 1.83, 95% CI: 1.06-3.17), especially those within the high-risk group (OR: 2.01, 95% CI: 1.03-3.94). 30-day morbidity outcomes showed black patients were more likely to remain in the hospital past 30 days, remain on mechanical ventilation past 30 days, experience an unplanned intubation, and experience a bleeding/transfusion complication. These disparities were especially prevalent within the high-risk group.
Discussion
Initial results from the study show mortality and morbidity disparities between black and white patients, namely at the high-risk level. These finding suggest that even after risk-stratifying patients based on their condition at birth, black patients still have worse postoperative outcomes. In the future, we aim to demonstrate race as a significant predictor of postoperative outcome in the CDHSG model, with the hope that greater resources and attention may be directed at those individuals who face a higher risk of mortality and postoperative complications.
-
PDF
-
Zoom