-
Author
Daniel Cordova -
PI
Breena Taira, MD, MPH
-
Co-Author
Tucker Avra, DVM; Jesus R. Torres, MD, MPH
-
Title
Advancing Language Access in the Emergency Department through Implementation Science: A Nursing Perspective
-
Program
Global Short-Term Training Program
-
Other Program (if not listed above)
-
Abstract
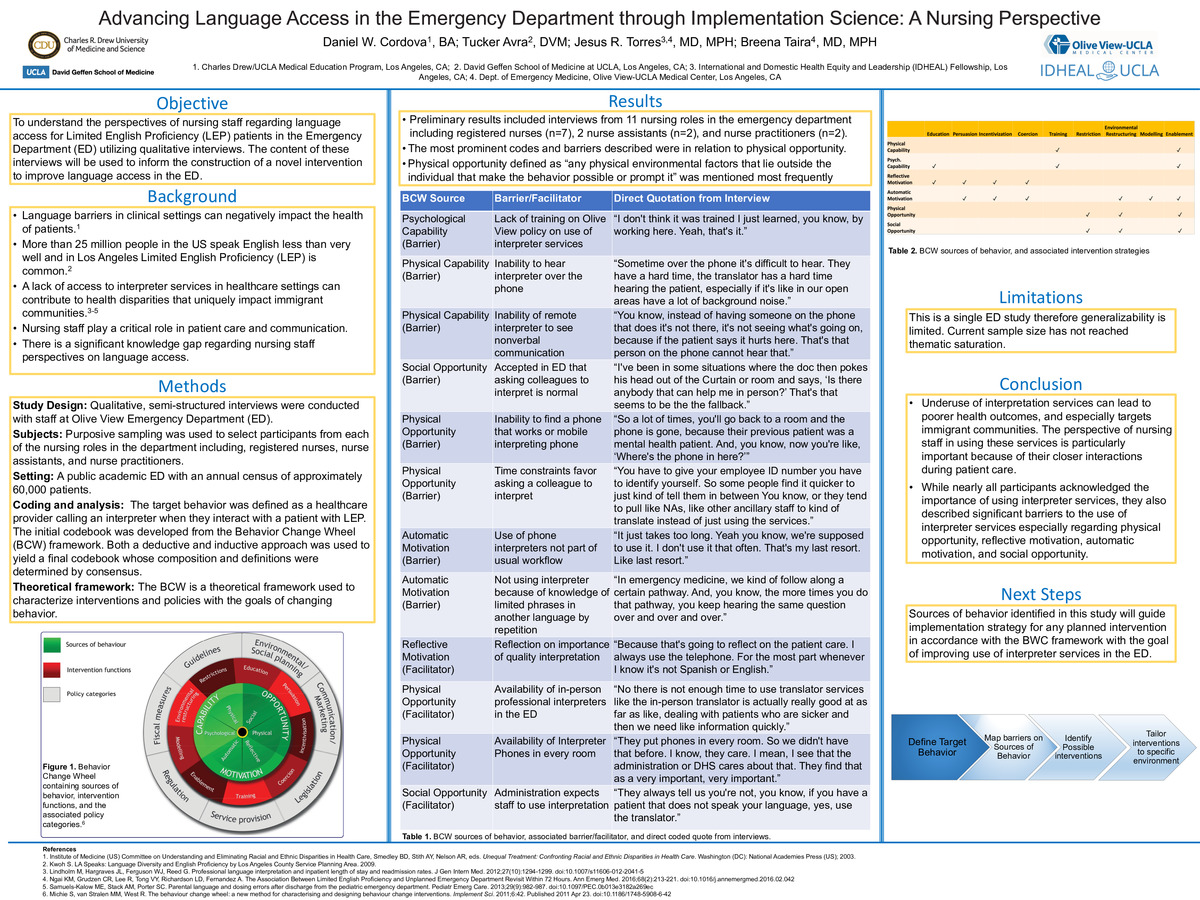
Background: Language barriers in clinical settings can negatively impact the health of patients.1 More than 25 million people in the US speak English less than very well, and in Los Angeles limited English proficiency (LEP) is common.2 A lack of access to interpreter services in healthcare settings can contribute to health disparities that uniquely impact immigrant communities.3-5 To date, efforts to increase rates of interpreter services use center on the physician’s perspective. There is a significant knowledge gap regarding the nursing perspective on the use of these services despite their important role in patient communication.
Objective: To understand the perspectives of nursing staff regarding language access for Limited English Proficiency (LEP) patients in the Emergency Department (ED). The content of these interviews will be used to inform the construction of a novel intervention to improve language access in the ED.
Methods:
Study design: A qualitative, single center study was conducted at Olive View-UCLA ED, with IRB approval of the Olive View/UCLA Education & Research Institute. Semi-structured, individual interviews were conducted with ED nursing staff.
Setting: A public academic ED with an annual census of approximately 60,000 patients. 58% of patients reporting to the ED requested an interpreter and 97% of those listed Spanish as the preferred language.
Subjects: Purposive sampling was used to select participants from each of the nursing roles in the department including, registered nurses, nurse assistants, and nurse practitioners. The final sample size will be determined when thematic saturation is reached.
Procedures: Interviews took place within the ED itself in private settings to avoid distraction and were recorded with participant consent using digital voice recorders. The audio recording from these sessions were transcribed and coded using Atlas.ti. The initial codebook was developed from the Behavior Change Wheel (BCW) framework. We took both a deductive and inductive approach to the data to yield a final codebook whose composition and definitions were determined by consensus.
Theoretical framework: The BCW is a theoretical framework used to characterize interventions and policies with the goals of changing behavior.6 The target behavior was defined as a healthcare provider calling an interpreter when they interact with a patient with LEP.
Results: Preliminary results included interviews from 11 ED staff members in nursing roles, including registered nurses (n=7), 2 nurse assistants (n=2), and nurse practitioners (n=2). Among these descriptions physical opportunity was the most frequently coded source of behavior followed by reflective motivation, automatic motivation, and social opportunity. A table providing a sample of identified barriers and facilitators matched to sources of behavior from the BCW is below.
BCW Source
Barrier/Facilitator
Direct Quotation from Interview
Psychological Capability
(Barrier)
Lack of training on Olive View policy regarding use of interpreter services
“I don't think it was a trained I just learned, you know, by working here. Yeah, that's it.”
Physical Capability
(Barrier)
Inability to hear interpreter over the phone
“Sometime over the phone it's difficult to hear. They have a hard time the translator has a hard time hearing the patient, especially if it's like in our open areas. Have a lot of background noise.”
Physical Capability
(Barrier)
Inability of remote interpreter to see nonverbal communication in the room
“You know, instead of having someone on the phone that does it's not there, it's not seeing what's going on, because if the patient says it hurts here. That's that person on the phone cannot hear that.”
Social Opportunity
(Barrier)
Accepted in ED that asking colleagues to interpret is normal
“I've been in some situations where the doc then pokes his head out of the Curtain or room and says, ‘Is there anybody that can help me in person?’ That's that seems to be the the fallback.”
Physical Opportunity
(Barrier)
Inability to find a phone that works or mobile interpreting phone
“So a lot of times, you'll go back to a room and the phone is gone, because their previous patient was a mental health patient. And, you know, now you're like, ‘Where's the phone in here?’”
Physical Opportunity
(Barrier)
Time constraints favor asking a colleague to interpret
Yeah for time? Yeah. You know, sometimes it takes a long time to, you know, you have to give your employee ID number you have to identify yourself. So some people find it quicker to just kind of tell them in between You know, or they tend to pull like NAs, like other ancillary staff to kind of translate instead of just using the services.
Automatic Motivation
(Barrier)
Use of phone interpreters not part of usual workflow
“It just takes too long. Yeah you know, we're supposed to use it. I don't use it that often. That's my last resort. Like last resort.”
Automatic Motivation
(Barrier)
Not using interpreter because of knowledge of limited phrases in another language by repetition
“In emergency medicine, we kind of follow along a certain pathway. And, you know, the more times you do that pathway, you keep hearing the same question over and over and over.”
Reflective Motivation
(Facilitator)
Reflection on importance of quality interpretation
“Because that's going to reflect on the patient care. I always use the telephone. For the most part whenever I know it's not Spanish or English”
Physical Opportunity
(Facilitator)
Availability of in person professional interpreters in the ED
“No there is not enough time to use translator services like the in person translator is actually really good at as far as like, dealing with patients who are sicker and then we need like information quickly.”
Physical Opportunity
(Facilitator)
Availability of Interpreter Phones in every room
“They put phones in every room. So we didn't have that before. I know, they care. I mean, I see that the administration or DHS cares about that. They find that as a very important very important”
Conclusions: While nearly all participants acknowledged the importance of using interpretation services with a patient that they do not speak the same language as, they also described significant barriers to the use of interpreter services especially with regard to physical opportunity, reflective motivation, automatic motivation, and social opportunity. Further work should be conducted to examine the barriers and facilitators that exist within these sources of behavior in order to identify possible intervention strategies.
References:
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US); 2003.
- Kwoh S. LA Speaks: Language Diversity and English Proficiency by Los Angeles County Service Planning Area. 2009.
- Lindholm M, Hargraves JL, Ferguson WJ, Reed G. Professional language interpretation and inpatient length of stay and readmission rates. J Gen Intern Med. 2012;27(10):1294-1299. doi:10.1007/s11606-012-2041-5
- Ngai KM, Grudzen CR, Lee R, Tong VY, Richardson LD, Fernandez A. The Association Between Limited English Proficiency and Unplanned Emergency Department Revisit Within 72 Hours. Ann Emerg Med. 2016;68(2):213-221. doi:10.1016/j.annemergmed.2016.02.042
- Samuels-Kalow ME, Stack AM, Porter SC. Parental language and dosing errors after discharge from the pediatric emergency department. Pediatr Emerg Care. 2013;29(9):982-987. doi:10.1097/PEC.0b013e3182a269ec
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. Published 2011 Apr 23. doi:10.1186/1748-5908-6-42
-
PDF
-
Zoom
https://uclahs.zoom.us/j/4041546639?pwd=OStERUYvMmdTN1pMVCtFVVF3QzRuQT09