-
Author
Lauren Taiclet -
PI
Ashley Feinsinger, Ph.D.
-
Co-Author
Nader Pouratian, MD, Ph.D.
-
Title
Patient-Participant Narratives of the Decision to Join Non-Therapeutic Intraoperative Neurophysiology Research: A Qualitative Analysis
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
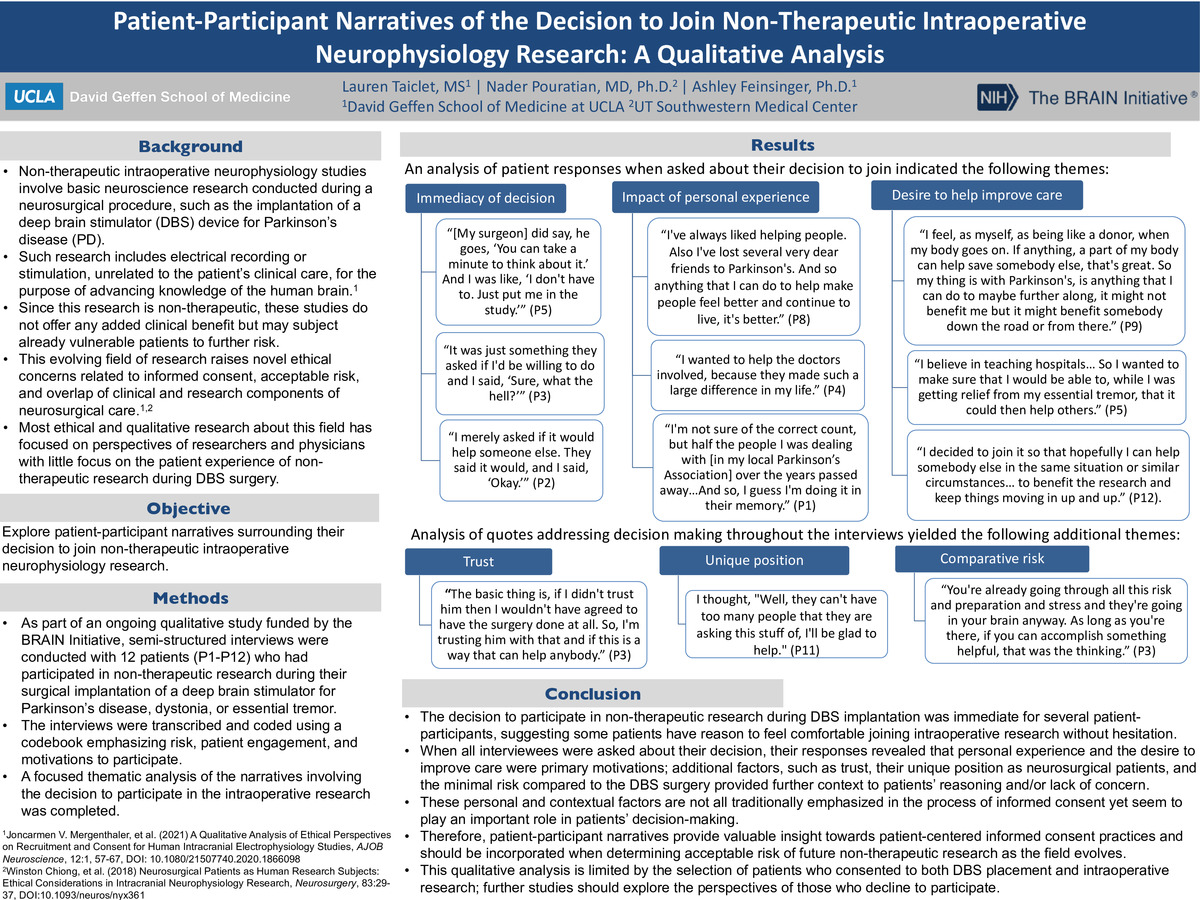
Background: Non-therapeutic intraoperative neurophysiology studies involve basic neuroscience research conducted during a neurosurgical procedure, such as the implantation of a deep brain stimulator (DBS) device for Parkinson’s disease (PD). Such research includes electrical recording or stimulation, unrelated to the patient’s clinical care, for the purpose of advancing knowledge of the human brain.1 Since this research is non-therapeutic, these studies do not offer any added clinical benefit but may subject already vulnerable patients to further risk. This evolving field of research raises novel ethical concerns related to informed consent, acceptable risk, and overlap of clinical and research components of neurosurgical care.1,2 Most ethical and qualitative research about this field has focused on perspectives of researchers and physicians with little focus on the patient experience of non-therapeutic research during DBS surgery.
Objective: Explore narratives of patient-participants about their decision to participate in non-therapeutic neurophysiology research during the surgical placement of a DBS device.
Methods: As part of an ongoing qualitative study funded by the BRAIN Initiative, semi-structured interviews were conducted with 12 patients who had participated in non-therapeutic research during their surgical implantation of a deep brain stimulator for Parkinson’s disease, dystonia, or essential tremor. The interviews were transcribed and coded using a codebook emphasizing risk, patient engagement, and motivations to participate. A focused thematic analysis of the narratives involving the decision to participate in the intraoperative research was completed.
Results: Thematic analysis of patient-participant responses when asked about their decision indicated the following themes: immediacy of decision, impact of personal experience on decision-making, and the desire to help improve clinical care. Analysis of the additional factors surrounding the decision to join yielded the following additional themes: trust in their surgeon or the institution, the unique position to be able to help as a DBS patient, and the minimal risk compared to the DBS surgery.
Conclusion: The decision to participate in non-therapeutic research during DBS implantation was immediate for several patient-participants, suggesting some patients have reason to feel comfortable joining intraoperative research without hesitation. When all interviewees were asked about their decision, their responses revealed that experience, either of their own illness or that of others, and the desire to improve care served as primary motivations. Additional factors, such as trust, their unique position as neurosurgical patients, and the minimal risk compared to the DBS surgery provided further context to patients’ reasoning and/or lack of concern. These personal and contextual factors are not all traditionally emphasized in the process of informed consent yet seem to play an important role in patients’ decision-making. Therefore, patient-participant narratives provide valuable insight towards patient-centered informed consent practices and should be incorporated when determining acceptable risk of future non-therapeutic research as the field evolves. This qualitative analysis is limited by the selection of patients who consented to both DBS placement and intraoperative research; further studies should explore the perspectives of those who decline to participate.
-
PDF
-
Zoom