-
Author
Karla Murillo -
PI
Anne L. Coleman MD, PhD
-
Co-Author
Ken Kitayama, MD and Fei Yu, PhD
-
Title
Geographical Barriers to Surgical Treatment for Cataracts and Glaucoma among Medicare Beneficiaries in Rural California
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
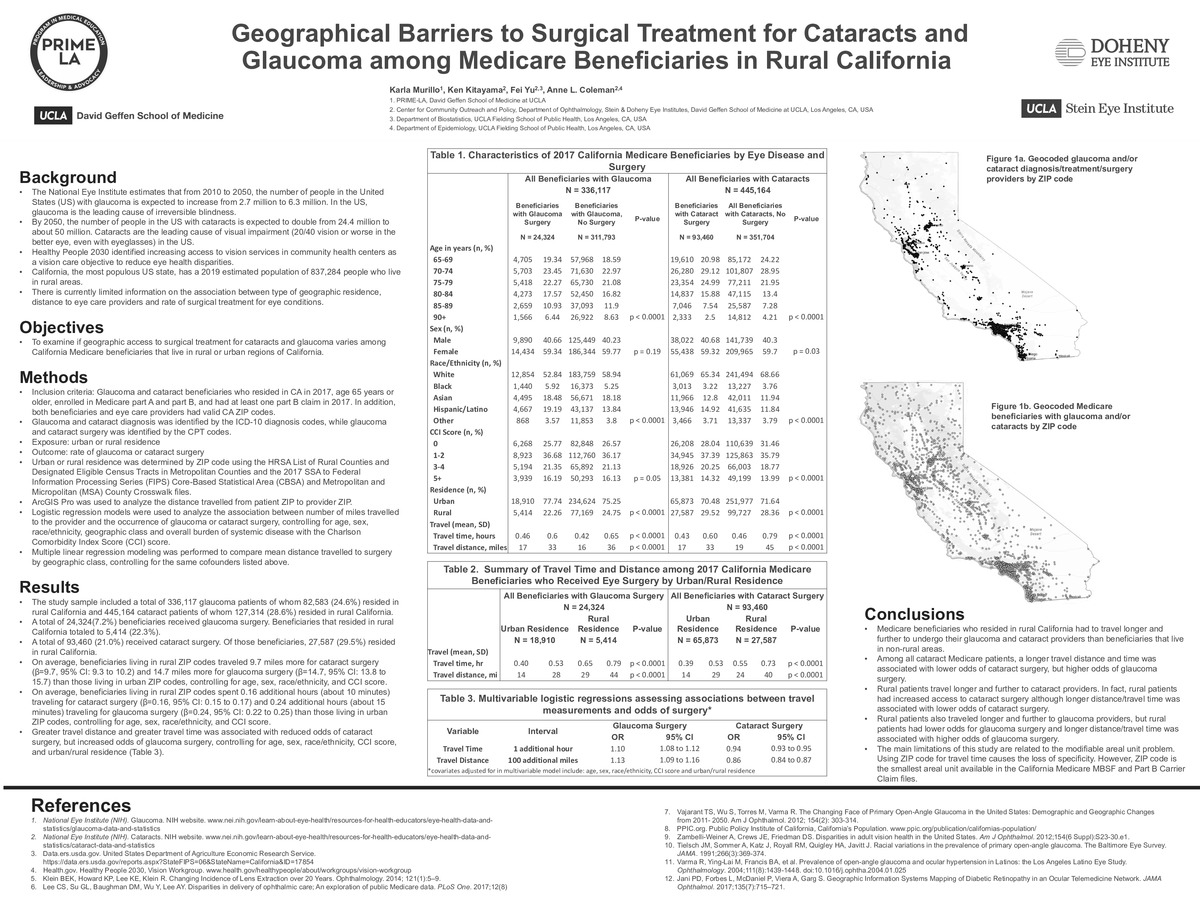
Purpose: To examine if geographic access to surgical treatment for cataracts and glaucoma varies among California Medicare beneficiaries that live in rural or urban regions of California.
Study design: Cross-sectional study
Methods: We analyzed data from a 100% sample of the 2017 California Medicare MBSF and Part B Carrier Claim files from the Centers for Medicare & Medicaid Services (CMS). The study population included all beneficiaries with a diagnosis of glaucoma or cataract based on ICD-10 diagnosis codes. Beneficiaries were included if they resided in CA in 2017, were 65 years or older, enrolled in Medicare part A and part B, and had at least one part B claim in 2017. In addition, both beneficiaries and eye care providers needed valid CA ZIP codes.
Urban or rural residence was determined by ZIP codes using the HRSA List of Rural Counties and Designated Eligible Census Tracts in Metropolitan Counties and the 2017 SSA to Federal Information Processing Series (FIPS) Core-Based Statistical Area (CBSA) and Metropolitan and Micropolitan (MSA) County Crosswalk files. Distance travelled to eye care providers was measured using ArcGIS Pro. Multiple linear regression models were performed to compare mean distance traveled to surgery by geographic class, controlling for age, sex, race/ethnicity and Charlson Comorbidity Index score. Multivariable logistic regression models were used to assess the effect of travel distance and time on the odds of receiving surgery.
Results: The study sample included 336,117 glaucoma patients of whom 82,583 (24.6%) resided in rural California and 445,164 cataract patients of whom 127,314 (28.6%) resided in rural California. A total of 24,324 (7.2%) glaucoma patients received glaucoma surgery and 93,460 (21.0%) cataract patients received cataract surgery. Beneficiaries who resided in rural California made up 5,414 (22.3%) of patients who received glaucoma surgery and 27,587 (29.5%) of cataract surgery patients. On average, after adjusting for potential confounders, beneficiaries living in rural ZIP codes traveled 9.7 miles more (β=9.7, 95% CI: 9.3 to 10.2) for cataract surgery and 14.7 miles more (β=14.7, 95% CI: 13.8 to 15.7) for glaucoma surgery than those living in urban ZIP codes, respectively. Moreover, among all cataract patients, for every additional 100 miles traveled, the odds of cataract surgery decreased by 14% (OR: 0.86, 95% CI: 0.84 to 0.87). However, the odds of glaucoma surgery increased by 13% (OR: 1.13, 95% CI: 1.09 to 1.16) for every additional 100 miles traveled among all glaucoma patients. For every additional hour of travel time, the odds of cataract surgery decreased by 6%, (OR: 0.94, 95% CI: 0.93 to 0.95) and the odds of glaucoma surgery increased by 10% (OR: 1.10, 95% CI: 1.08 to 1.12).
Conclusions: In 2017, Medicare beneficiaries who resided in rural areas of California had to travel longer and further to undergo their cataract and glaucoma surgery than beneficiaries who lived in non-rural areas. Among all cataract Medicare patients, a longer travel distance and time was associated with lower odds of cataract surgery. On the other hand, among all glaucoma patients, a longer travel distance and time was associated with higher odds of glaucoma surgery. Further studies are needed to understand such complex relationships for different types of eye surgery.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/91837022982?pwd=OURLVUFqMllDYUdndFdOenRWS1Zndz09