-
Author
Bryan Vuong -
PI
Catherine A. Sarkisian, MD, MSHS
-
Co-Author
Richard K. Leuchter, MD; Chad Wes A. Villaflores, MS; Sitaram Vangala, MS; Catherine A. Sarkisian, MD, MSHS
-
Title
Financial Impact of Racial Disparities in Potentially Avoidable Hospitalizations during the Covid-19 Pandemic
-
Program
Internal Medicine Chief's Fellowship
-
Other Program (if not listed above)
-
Abstract
Background:
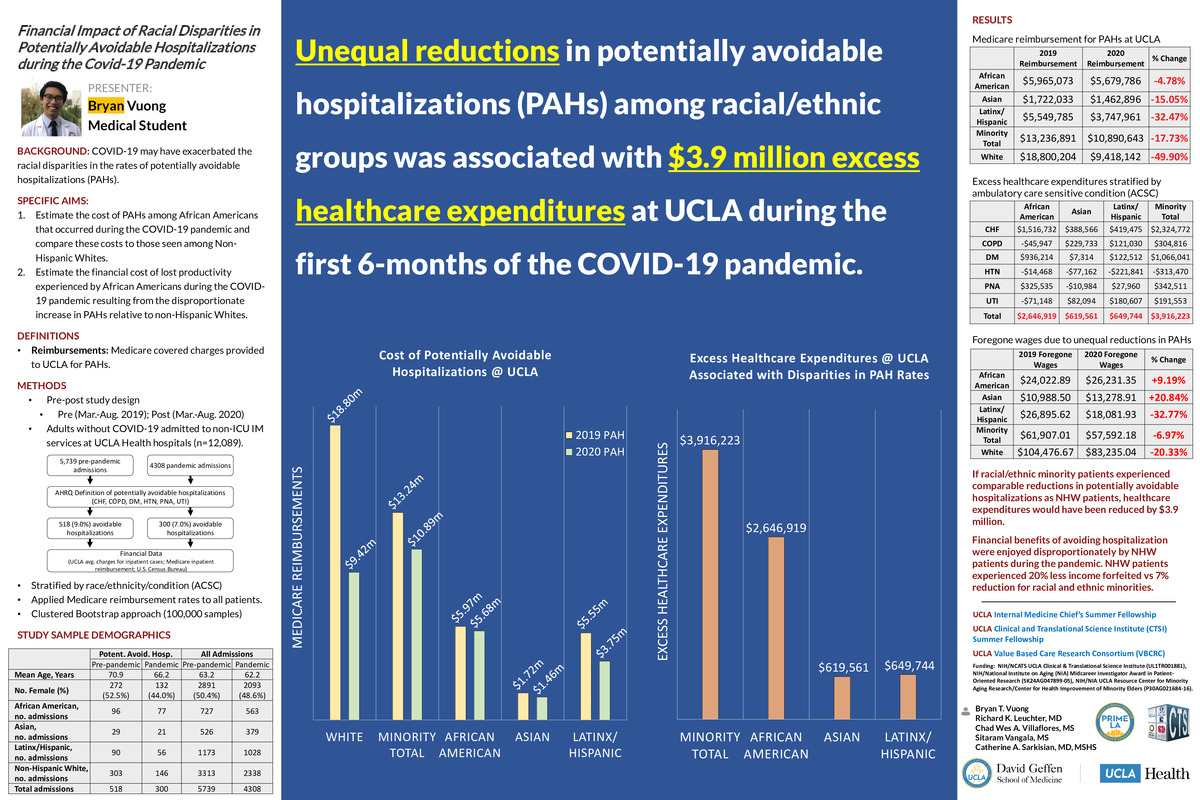
There is a growing body of evidence describing racial disparities in potentially avoidable hospitalizations to suggest that vulnerable and underserved patient populations experience disproportionately higher barriers to accessing outpatient care, worse health outcomes, and greater financial burden. While the racial and ethnic disparities in potentially avoidable hospitalizations pre-date the coronavirus disease 2019 (COVID-19) pandemic, recent findings from Leuchter et al. suggest that COVID-19 has exacerbated the disparities in the rates of potentially avoidable hospitalizations for African Americans compared to non-Hispanic Whites. A greater understanding of the economic implications of these findings is an important step in reducing this disparity.
Objective:
We aim to quantify the financial impact that unequal reductions in potentially avoidable hospitalizations have on both the healthcare system and African American patients within UCLA in the following ways:
Aim 1: Estimate the cost of potentially avoidable hospitalizations among African Americans that occurred during the COVID-19 pandemic and compare these costs to those seen among Non-Hispanic Whites.
Aim 2: Estimate the financial cost of lost productivity experienced by African American patients during the COVID-19 pandemic resulting from the disproportionate increase in potentially avoidable hospitalizations relative to non-Hispanic Whites.
Methods:
This pre-post study included patients admitted to any UCLA Health hospital for a potentially avoidable hospitalization between March 15 - August 31 of 2019 (pre) and March 15 - August 31 of 2020 (post). Changes in the number of potentially avoidable hospitalizations, as defined by the Agency for Healthcare Research and Quality (AHRQ) guidelines for ambulatory care sensitive conditions, were calculated using a cluster bootstrap approach and stratified by race and ethnicity. Excess healthcare expenditures were estimated from the difference in potentially avoidable hospitalizations between non-Hispanic White and African American patients, and the median expenditure per admission was based on publicly available Medicare reimbursement rates. Lost productivity followed the human capital approach and estimated the indirect cost of absenteeism from patients’ length of stay and daily wage.
Results:
Between March 15 and August 31, 2020, 300 out of 4308 hospitalizations (7.0%) were potentially avoidable, whereas 518 of 5739 (9.0%) hospitalizations were potentially avoidable in the same 6-month period of 2019. During this time, potentially avoidable hospitalizations for non-Hispanic Whites decreased 50.3% (95% CI, 41.4 - 60.9), compared to African Americans who saw a decrease of 8.0% (95% CI, -16.2 - +39.4). If African Americans experienced the same reductions in potentially avoidable hospitalizations as did non-Hispanic Whites, expenditures would have been reduced by $2,646,919 during the first 6-months of the COVID-19 pandemic. For lost productivity, non-Hispanic Whites experienced a 20.3% reduction ($104,477 in 2019; $83,235 in 2020) of foregone wages compared to African Americans who experienced an increase of 9.2% ($24,023 in 2019; $26,231 in 2020) in foregone wages in the first 6 months of the COVID-19 pandemic.
In an exploratory analysis we found that if the decreases in potentially avoidable hospitalizations for non-Hispanic Whites were experienced by Asian and Latinx patients to the same extent, expenditures would have been reduced by an additional $1,269,305 ($619,561 and $649,744, respectively). Furthermore, Asian and Latinx patients experienced an increase of 20.8% and decrease of 32.8% of foregone wages, respectively. Taken together, African American, Asian and Latinx patients collectively experienced a reduction of 7.0% of foregone wages in the first 6 months of the COVID-19 pandemic.
Conclusions:
If racial/ethnic minority patients experienced comparable reductions in potentially avoidable hospitalizations as non-Hispanic White patients, expenditures would have been reduced by $3.9 million during the first 6-months of the COVID-19 pandemic. Additionally, we found that the financial benefits of avoiding hospitalization were enjoyed disproportionately by non-Hispanic White patients compared to racial/ethnic minority patients in the first 6-months of the pandemic. These findings further inform the need to develop interventions and policies to combat these disparities.
References:
1. O'Neil SS, Lake T, Merrill A, Wilson A, Mann DA, Bartnyska LM. Racial disparities in hospitalizations for ambulatory care-sensitive conditions. Am J Prev Med. 2010 Apr;38(4):381-8. doi: 10.1016/j.amepre.2009.12.026. PMID: 20307806.
2. Pappas G, Hadden WC, Kozak LJ, Fisher GF. Potentially avoidable hospitalizations: inequalities in rates between US socioeconomic groups. Am J Public Health. 1997;87(5):811-816. doi:10.2105/ajph.87.5.811
3. Feng C, Paasche-Orlow MK, Kressin NR, et al. Disparities in Potentially Preventable Hospitalizations: Near-National Estimates for Hispanics. Health Serv Res. 2018;53(3):1349-1372. doi:10.1111/1475-6773.12694
4. Leuchter RK, Villaflores CWA, Norris KC, Sorensen A, Vangala S, Sarkisian CA. Racial Disparities in Avoidable Hospitalizations During the COVID-19 Pandemic. Am J Prev Med. 2021. In Press.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/94508222440?pwd=TUErUXQweVNmMnlGZldaVDI4NVBRdz09