-
Author
Jasmine Deng -
PI
Fady Kaldas, MD
-
Co-Author
Daisuke Noguchi, MD, PhD; Minah Ha, BS; Vatche Agopian, MD; Douglas Farmer, MD
-
Title
Outcomes in Simultaneous Liver-Kidney Transplantation Compared to Liver Transplantation Alone and Kidney Transplantation After Liver Transplantation
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
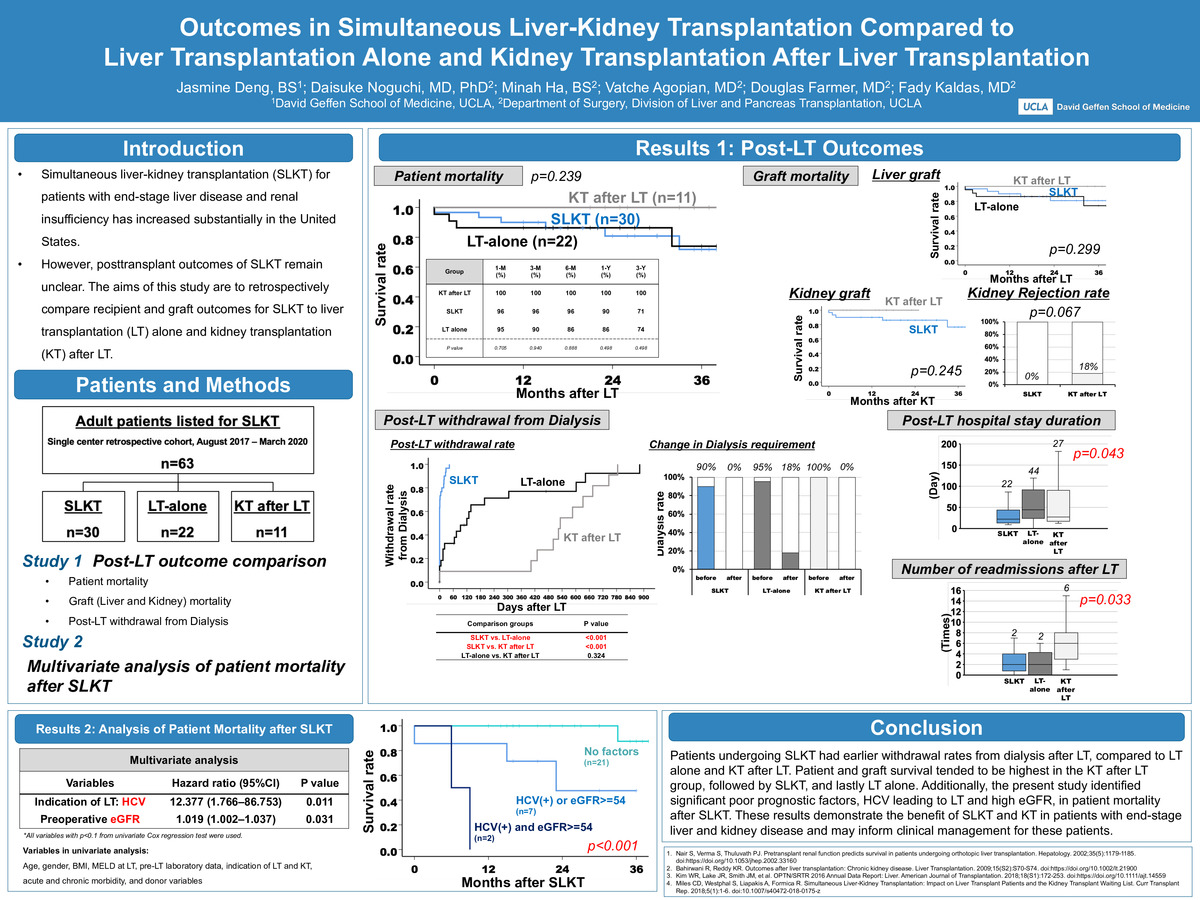
Objective: To examine and compare the outcomes of liver transplantation patients with renal failure who were listed for simultaneous liver-kidney transplantation since August 2017 at the University of California, Los Angeles.
Background: Renal dysfunction prior to liver transplantation (LT) is associated with decreased survival and kidney disease post-transplantation.1 Chronic kidney disease (CKD) after transplantation is a major complication affecting mortality post-transplantation, particularly in patients who remain on dialysis after LT.2 Since the implementation of the Model for End-Stage Liver Disease (MELD) score for donor allocation in 2002, there has been a substantial increase in the number of simultaneous liver-kidney transplantations (SLKT) performed in the United States.3 The revised Organ Procurement and Transplantation Network (OPTN) policy, implemented in August 10th, 2017, outlines and standardizes the medical eligibility for candidates to receive SLKT. This policy provided a “safety net” option to prioritize all LT recipients in the kidney allocation system in the case that they continue to undergo dialysis or have persistent kidney dysfunction after LT.4 However, there is still little known the groups affected by these policies: patients undergoing SLKT, receiving isolated liver, or receiving KT after LT with priority on the safety net. In this study, we have incorporated the safety net option and examined patient outcomes and graft survival among high-acuity patients who received SLKT, patients who were listed for SLKT but received LT alone, and those who were listed for SLKT but received KT after LT.4
Methods: Patients undergoing LT at UCLA since August 2017 were identified using a transplant database. A retrospective chart review was performed to identify and categorize patients listed for SLKT into subgroups: patients undergoing SLKT, LT alone, KT after LT. Several variables were collected, including demographic and comorbidity information for recipients and donors, etiology of liver and kidney disease, duration and renal dysfunction and failure, dialysis status and duration, MELD at LT, laboratory values, re-admissions, septic episodes, discharge location, and vasopressor requirements.
Continuous variables were expressed as median and interquartile range and were compared using the Mann-Whitney U test for 2-group. Categorical variables were compared using the chi-square test or Fisher exact test for 2-group and the Kruskal-Wallis test for 3-group comparison. Survival curves for patient and graft survival were computed using the Kaplan-Meier method, and p values for group comparison including SLKT, LT alone, and KT after LT were computed using the log-rank test. We performed univariate and multivariate analyses to detect risk factors for overall survival in patients with SLKT using the Cox regression model. All tests were 2-sided, the significance level was p< 0.05, and the confidence interval (CI) was determined at 95%. All analyses were performed using SPSS Statistics version 27 (IBM Corporation).
Results: 63 adult patients listed for SLKT met inclusion criteria. 30 patients received SLKT, 22 received LT alone, and 11 received KT after LT. Two major analyses were performed: a comparison of post-LT outcomes and a multivariate analysis of SLKT patient mortality. Although the difference of patient survival rate was not significant (p=0.239), KT after LT patients had the highest survival rate, followed by SLKT patients, and lastly patients receiving LT alone (3 month: 100% vs. 96% vs. 90%, 1 year: 100% vs. 90%vs. 86%, 3 year: 100% vs. 71% vs. 74%). There were no patient deaths nor liver or kidney graft failures in the KT after LT group. The liver and kidney graft mortality results followed the same trend, although the difference was not significant (p=0.299 comparing the three groups and p=0.245 comparing the KT after LT and SLKT groups). Although the KT after LT group was noted to have higher kidney graft survival, this group had a 15% kidney rejection rate compared to 0% for the SLKT group (p=0.067).
We also compared the post-LT withdrawal from dialysis rates and change in dialysis requirements among the three groups. The SLKT group had the shortest withdrawal time from dialysis and perfectly recovered from dialysis (90% before SLKT to 0% after SLKT). The KT after LT group had the longest withdrawal time from dialysis but all patients recovered from dialysis (100% before KT to 0% after KT). The LT alone group required a longer dialysis withdrawal time compared to SKLT and did not achieve 100% dialysis recovery (95% before LT to 18% after LT). Differences in post-LT withdrawal rates from dialysis were statistically significant between SLKT vs. LT alone groups and SLKT vs. KT after LT groups (both p=<0.001), whereas there was no significant difference between groups of LT alone and KT after LT (p=0.324). Additionally, the SLKT group had the shortest median post-LT hospital stay compared to the other groups (22 days vs. 44 days vs. 27 days, p=0.043). The SLKT group also had the lowest median number of readmissions after LT among the three groups (2 times vs. 2 times vs. 6 times, p=0.033).
A univariate analysis was performed using the following variables: age, gender, BMI, MELD score at LT, pre-LT laboratory data, indication of LT and KT, acute and chronic morbidity such as mechanical ventilation, vasopressor requirement, dialysis requirement, length of dialysis and renal failure, and donor variables. A multivariate analysis for survival outcomes of patients with SLKT was performed using the variables with p < 0.1 in a univariate analysis. The analysis detected hepatitis C (HCV) leading to LT and high preoperative eGFR as the significant poor prognostic risk factors (p=0.011 and p=0.031, respectively). Patients with SLKT were categorized into three groups based on the risk factors (HCV or not, eGFR ≥ 54 or eGFR < 54). Patients with neither HCV nor high eGFR (n=21) had the highest survival rates followed by patients with either HCV or high eGFR (n=7), while patients with both HCV and high eGFR (n=2) were noted to have the lowest survival (p=<0.001).
Conclusions: In this single-center retrospective study, patients undergoing SLKT had earlier withdrawal rates from dialysis after LT, compared to LT alone and KT after LT. Patient and graft survival tended to be highest in the KT after LT group, followed by SLKT, then followed by LT alone. Additionally, the present study identified significant poor prognostic factors, HCV leading to LT and high eGFR, in patient mortality after SLKT. These results demonstrate the benefit of SLKT and KT in patients with end-stage liver and kidney disease and may inform clinical management for these patients.
References:
- Nair S, Verma S, Thuluvath PJ. Pretransplant renal function predicts survival in patients undergoing orthotopic liver transplantation. Hepatology. 2002;35(5):1179-1185. doi:https://doi.org/10.1053/jhep.2002.33160
- Bahirwani R, Reddy KR. Outcomes after liver transplantation: Chronic kidney disease. Liver Transplantation. 2009;15(S2):S70-S74. doi:https://doi.org/10.1002/lt.21900
- Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2016 Annual Data Report: Liver. American Journal of Transplantation. 2018;18(S1):172-253. doi:https://doi.org/10.1111/ajt.14559
- Miles CD, Westphal S, Liapakis A, Formica R. Simultaneous Liver-Kidney Transplantation: Impact on Liver Transplant Patients and the Kidney Transplant Waiting List. Curr Transplant Rep. 2018;5(1):1-6. doi:10.1007/s40472-018-0175-z
-
PDF
-
Zoom
https://uclahs.zoom.us/j/97971674250?pwd=TkhOVHRkayt1disvd21lcXdWb1JNUT09