-
Author
Sara Pena Carmona -
PI
Arpan Patel MD PhD
-
Co-Author
Gery Ryan PhD, Diana Tisnado PhD, Anne Walling MD PhD, Neil Wenger MD MPH
-
Title
Palliative Needs of Patients with Decompensated Cirrhosis Being Considered for Liver Transplantation
-
Program
Other
-
Other Program (if not listed above)
-
Abstract
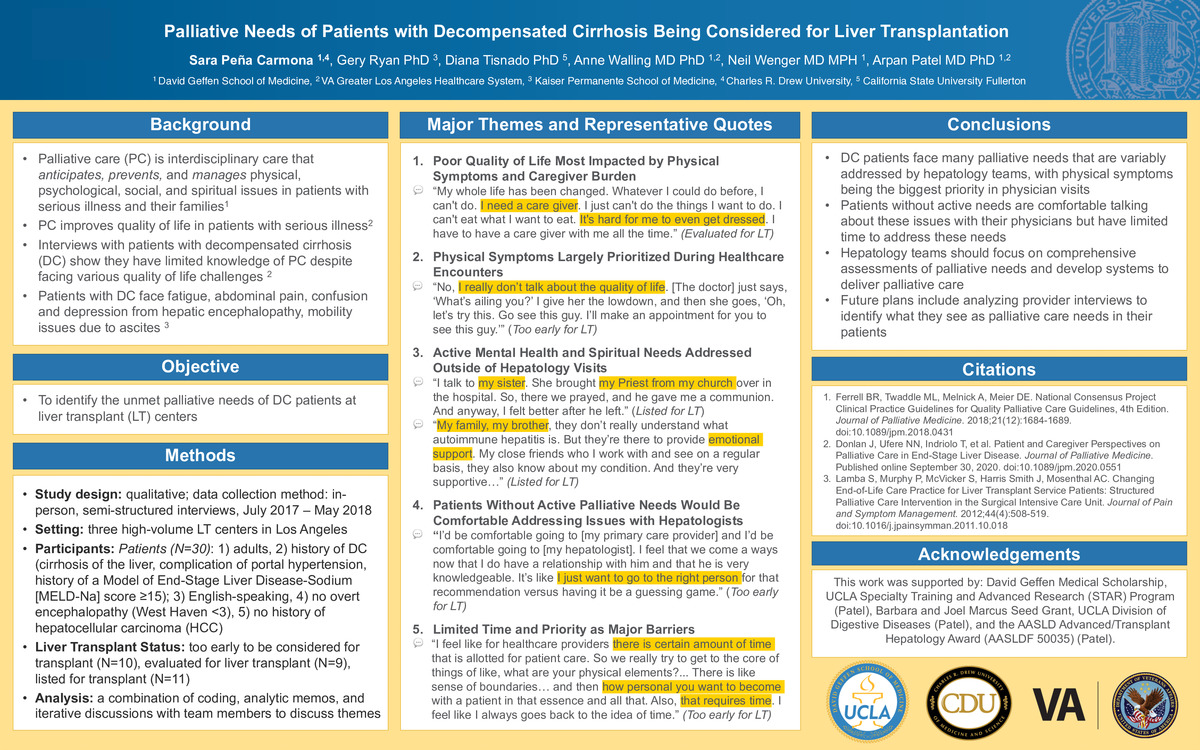
Background:
Palliative care (PC) is interdisciplinary care which anticipates and manages physical, psychological, social, and spiritual issues for patients with serious illness, their families, and their caregivers to improve their quality of life (1). While palliative care is becoming more integrated in the care of patients with serious illnesses, interviews with end-stage liver disease (ESLD) and their caregivers have shown their knowledge of PC is limited despite facing debilitating quality of life challenges (2,3). This project aims to examine the unmet palliative needs of patients with decompensated cirrhosis (DC) being considered for liver transplant (LT).
Methods:
We performed semi-structured interviews with patients with DC at three high-volume LT centers in Los Angeles from July 2017- May 2018. DC was defined as a history of cirrhosis, a complication of portal hypertension, and history of MELD-Na ≥15. Participants were all English-speaking adults with a history of DC, no overt encephalopathy, and no history of hepatocellular carcinoma. Interviews of patients too early (N=10), evaluated (N=9), or listed (N=11) for liver transplant were analyzed for major themes. This was performed using a combination of coding, analytic memos, and iterative discussions among team members.
Results:
Interviews showed five major domains of palliative needs and perceptions among patients: symptom burden and management, mood issues, caregiver burden, spiritual needs, and interactions with healthcare providers. Quality of life was poor overall, and several palliative needs were identified, with physical symptoms and caregiver burden being most impactful in patient’s lives. During encounters with healthcare teams, addressing physical symptoms was largely prioritized. Patients with active mental health and spiritual needs were addressed these issues outside hepatology visits. Patients without active palliative needs felt comfortable addressing these issues with hepatologists. Limited time and priority during physician encounters were seen as major barriers by patients in addressing palliative needs during clinic.
Conclusions:
DC patients faced multiple palliative care needs that were variably addressed by hepatology teams. Healthcare visits prioritized physical symptom burden and management. While patients felt comfortable addressing palliative care needs with their hepatologists, they have a limited time to address these needs. Hepatology teams should focus on comprehensive palliative needs assessments and developing systems for palliative care delivery.
Sources:
1. Ferrell BR, Twaddle ML, Melnick A, Meier DE. National Consensus Project Clinical Practice Guidelines for Quality Palliative Care Guidelines, 4th Edition. Journal of Palliative Medicine. 2018;21(12):1684-1689. doi:10.1089/jpm.2018.0431
2. Donlan J, Ufere NN, Indriolo T, et al. Patient and Caregiver Perspectives on Palliative Care in End-Stage Liver Disease. Journal of Palliative Medicine. Published online September 30, 2020. doi:10.1089/jpm.2020.0551
3. Lamba S, Murphy P, McVicker S, Harris Smith J, Mosenthal AC. Changing End-of-Life Care Practice for Liver Transplant Service Patients: Structured Palliative Care Intervention in the Surgical Intensive Care Unit. Journal of Pain and Symptom Management. 2012;44(4):508-519. doi:10.1016/j.jpainsymman.2011.10.018
-
PDF
-
Zoom
https://uclahs.zoom.us/j/92642542090?pwd=Mm5qQkFiNExSL0xDSDJsK0NrWkNkQT09