-
Author
Melissa Yao -
PI
David Sarraf, MD
-
Co-Author
JooYeon Jung, MD, Stacy Pineles, MD, Laura Bonelli, MD
-
Title
Using Optical Coherence Tomography and Optical Coherence Tomography Angiography to Understand Pathoanatomical Changes of the Vitreoretinal Interface and Inner Retina in Patients with Neurofibromatosis 2
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
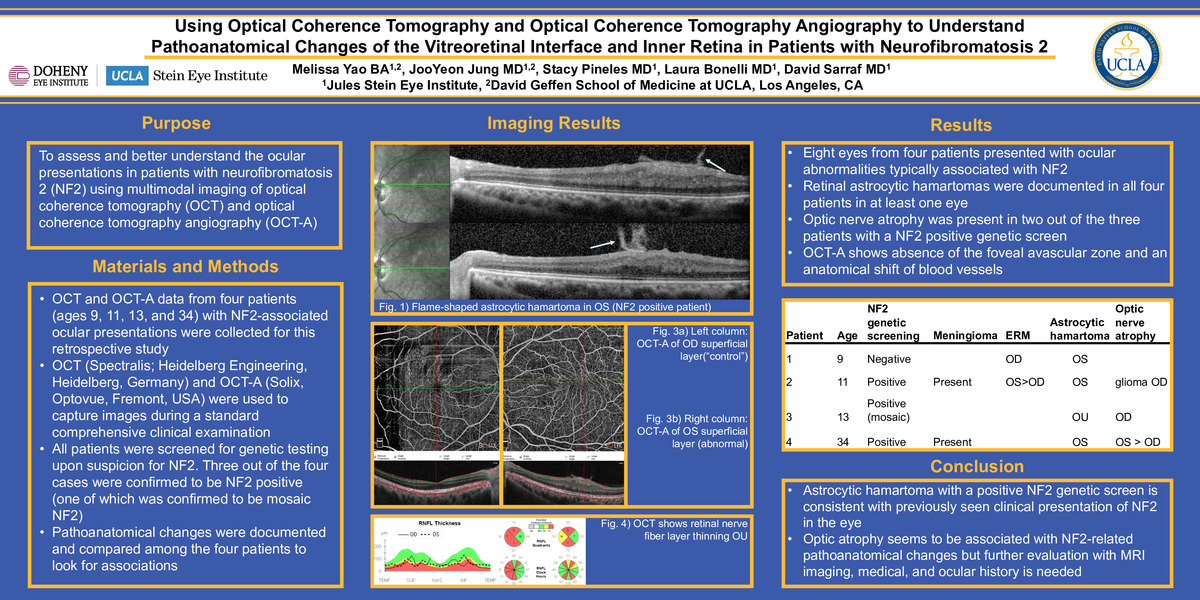
Introduction: Neurofibromatosis 2 (NF2) is a genetic disorder caused by inactivating mutations of the NF2 gene on chromosome 22q. The NF2 gene is a tumor suppressor gene that codes for a protein named Merlin, also known as neurofibromin 2. Merlin has been shown to be strongly expressed in controlling growth in the ciliary margin (CM) and retinal pigment epithelium (RPE) regions of the eye. Thus, the loss of NF2 results in hyperplasia in these regions and the consequent ocular abnormalities seen in patients with NF2. The prevalence of NF2 is about 1 in 60,000 and is characterized by multiple central and peripheral nervous system tumors, bilateral vestibular schwannomas, and ocular manifestations.
Purpose: We want to assess and better understand the ocular presentations in patients with neurofibromatosis 2 (NF2) by using multimodal imaging including optical coherence tomography (OCT) and optical coherence tomography angiography (OCT-A).
Methods: Data from four patients (three pediatric and one adult) with NF2-associated ocular presentations were collected for this retrospective study. OCT (Spectralis, Heidelberg, Germany) and OCT-A (Solix, Optovue, Fremont, USA) data were collected during standard comprehensive clinical exams. Images with low quality scores (Q score < 5/10) were excluded. OCT-A data were collected from three out of the four patients and results are pending for the fourth patient. All patients were screened for NF2 given other medical history. Three out of the four patients were confirmed to be NF2 positive, of which one has mosaic NF2. Pathoanatomical changes were evaluated, analyzed and compared among the four patients.
Results: All eight eyes from four patients presented with ocular abnormalities typically associated with NF2. Retinal flame-shaped astrocytic hamartomas were present in at least one eye in every patient as expected. Meningiomas were documented in two of the three NF2 positive patients. Optic nerve atrophy was also present in two out of the three NF2 positive patients. Preliminary OCT-A images show the absence of the foveal avascular zone and an anatomical shift of blood vessels in eyes with astrocytic hamartomas.
Conclusions: The characteristic astrocytic hamartoma at the vitreoretinal interface along with a positive NF2 genetic screen is consistent with previously described NF2 clinical presentation. We also document the presence of optic atrophy and hypothesize that the pathology may be the result of meningioma compression on the optic nerve. Further evaluation with MRI imaging, medical, and ocular history will be needed to evaluate the possible association of optic atrophy with NF2.
-
PDF
-
Zoom