-
Author
Mengdong He -
PI
Seoyoung C. Kim, MD, ScD, MSCE
-
Co-Author
Yvonne C. Lee, MD, MMSc, Yinzhu Jin, MS, Rishi J. Desai, PhD, Seanna M. Vine, MPH
-
Title
Impact of Initiation of Biologic and Targeted Synthetic Disease-Modifying Antirheumatic Drugs on Pain Medication Use in Patients With Rheumatoid Arthritis
-
Program
Other
-
Other Program (if not listed above)
Medical and Graduate Student Preceptorship, Rheumatology Research Foundation
-
Abstract
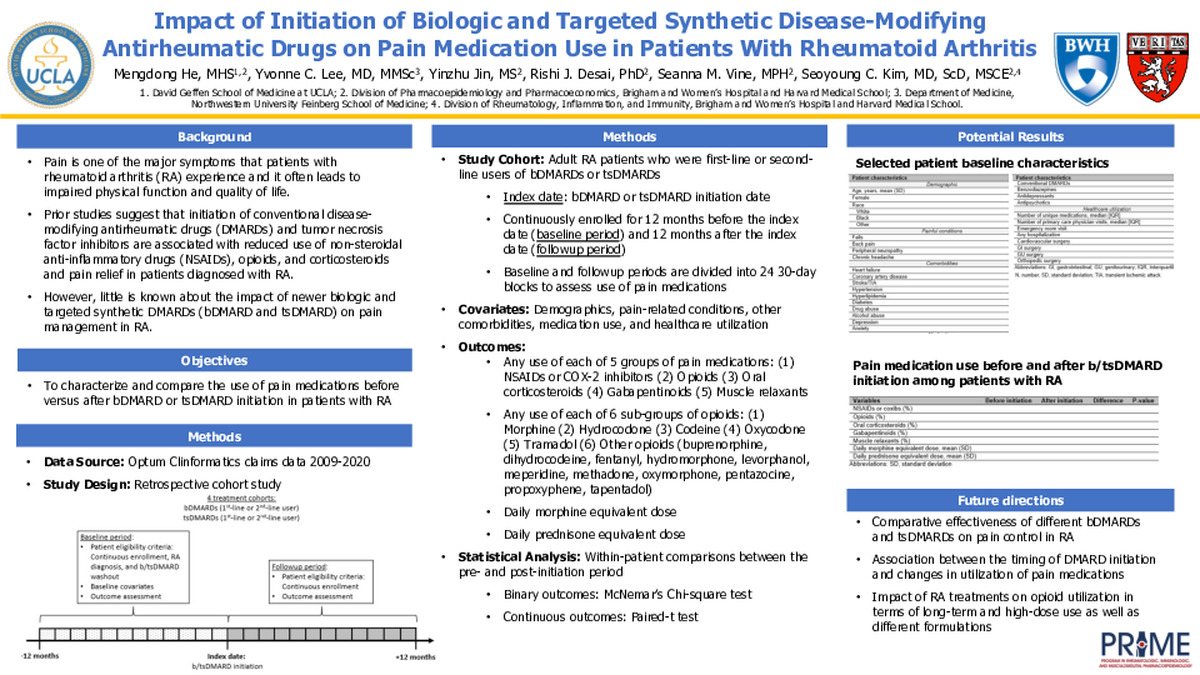
Background: Pain is one of the major symptoms that patients with rheumatoid arthritis (RA) experience and it often leads to impaired physical function and quality of life. Prior studies suggest that initiation of conventional disease-modifying antirheumatic drugs (DMARDs) and tumor necrosis factor inhibitors are associated with reduced use of non-steroidal anti-inflammatory drugs (NSAIDs), opioids, and corticosteroids and pain relief in patients diagnosed with RA. However, little is known about the impact of newer biologic and targeted synthetic DMARDs (bDMARD and tsDMARD) on pain management in RA.
Objective: To characterize and compare the use of 5 groups of pain medications (i.e., NSAIDs or COX-2 inhibitors, opioids, oral corticosteroids, gabapentinoids, and muscle relaxants) before versus after bDMARD or tsDMARD initiation in patients with RA.
Methods: We retrospectively identified 4 cohorts of adult RA patients who were first-line or second-line users of bDMARDs or tsDMARDs in the Optum Clinformatics claims data (2009-2020). The first-line users had no prior dispensing of any bDMARDs or tsDMARDs any time prior to the cohort entry (i.e. bDMARD or tsDMARD initiation date) while the second-line users had prescriptions of other bDMARDs or tsDMARDs before initiation of the index DMARD (using a washout period of 12 months). Patients were required to have ≥12 months of continuous insurance enrollment before and after the cohort entry. Those who had pregnancy, cancer, kidney transplant, or dialysis during the baseline period, or initiated more than one bDMARD or tsDMARD at the cohort entry were excluded. Our primary outcome is any use of each of the 5 groups of pain medications. Secondary outcomes include any use of each of 6 sub-groups of opioids (i.e., morphine, hydrocodone, codeine, oxycodone, tramadol, and other opioids). Among those who used opioids and oral corticosteroids, we also calculated their daily morphine equivalent dose and daily prednisone equivalent dose during the study period. Using intention-to-treat analysis, the study participants were followed from one day after the cohort entry through 12 months. Within-patient differences between the pre- and post-initiation period are compared using McNemar’s Chi-square test and paired-t test for binary and continuous outcomes, respectively.
Future Directions: Understanding of the impact of different bDMARDs and tsDMARDs on pain control in RA patients would help guide clinical decision-making regarding the initiation of RA treatments and use of co-therapies. It would also help RA patients to achieve optimal symptom control, minimize use of pain medications with risk of addiction, abuse and overdose such opioids, and improve overall quality of life. For next steps, we may assess the comparative effectiveness of different bDMARDs and tsDMARDs on pain control in RA and the association between the timing of DMARD initiation and changes in utilization of pain medications. We may also further examine the impact of RA treatments on opioid utilization in terms of long-term and high-dose use as well as different formulations.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/98437519380?pwd=aW1YbDhsL0ZKU2xtR1daQVpsOVQ0QT09