-
Author
Callie Cuff -
PI
Lin Chang, M.D.
-
Co-Author
Swapna Joshi, Nancee Jaffe, Lisa Lin, Cathy Liu, Janelle Smith, Cory Tripp, Rachel Sarnoff, Rusha Modi
-
Title
Fructose Reintroduction in Irritable Bowel Syndrome Patients Successfully Treated with a low FODMAP diet
-
Program
Internal Medicine Chief's Fellowship
-
Other Program (if not listed above)
-
Abstract
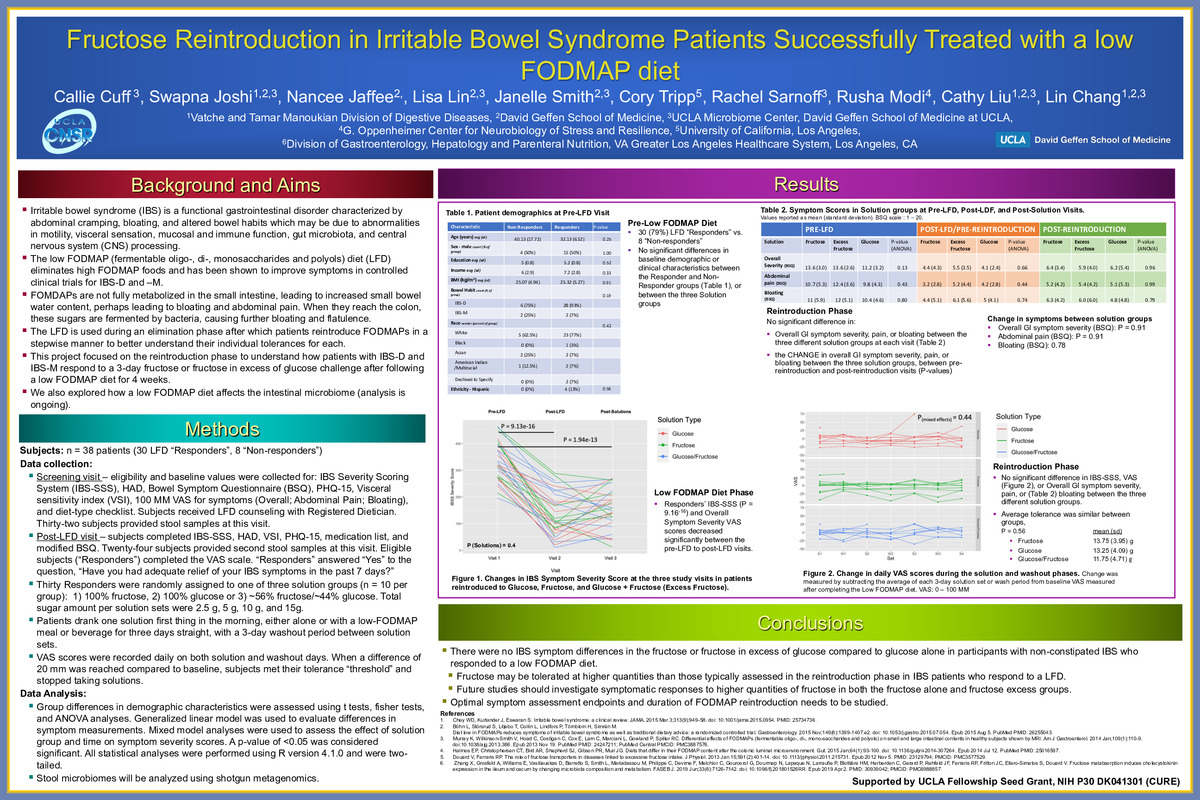
Background The low FODMAP (fermentable oligo-, di-, monosaccharides and polyols) diet (LFD) has been shown to improve symptoms in controlled clinical trials for patients with IBS with diarrhea (IBS-D) or IBS with mixed bowel habits (IBS–M). The LFD eliminates high FODMAP-containing foods from the diet for about 4 weeks, after which patients empirically reintroduce each major FODMAP to better understand their individual tolerances. However, the optimal protocol to reintroduce FODMAPS and assess the tolerance to each major FODMAP group in IBS patients who respond to an LFD has not been well studied.
Objectives To compare subjective overall severity ratings to solutions with increasing amounts of fructose, fructose in excess of glucose, and glucose in patients with IBS-D or IBS-M who have responded to a LFD. To compare stool microbiome profiles of participants with IBS who did or did not experience adequate relief from the LFD.
Methods Data were obtained from 38 participants who completed a four-week LFD intervention. Clinical symptom questionnaires and stool samples were collected at visits before and after the LFD phase. Following the LFD stage, 30 (79%) subjects were deemed LFD “Responders” and 8 subjects as “non-Responders.” Responders were randomly assigned to one of three solution groups: 1) 100% fructose, 2) 100% glucose or 3) ~56% fructose/~44% glucose. Subjects ingested four solution sets of increasing sugar content for three consecutive mornings, with a 3-day washout period between sets. Daily VAS scores obtained on solution and washout days. The primary endpoint was mean change in overall symptom severity VAS at the last solution compared to baseline scores determined after completing the LFD. Other secondary endpoints explored were IBS Symptom Severity Scale (IBS-SSS), HAD, Bowel Symptom Questionnaire (BSQ), PHQ-15, and Visceral sensitivity index (VSI).
Statistical analyses were performed using R version 4.1.0 to assess group differences in demographic characteristics, differences in symptom measurements, and the effect of solution group and time on symptom severity scores. Stool microbiomes will be analyzed using shotgun metagenomics.
Results Responders’ IBS-SSS and Overall Symptom Severity VAS scores decreased significantly (P = 9.16-16) between the pre-LFD to post-LFD visits. Following the reintroduction phase, there was not a statistically significant difference in the changes of VAS (Overall GI symptom severity), IBS-SSS, or BSQ (Overall GI symptom severity, pain, bloating), between the three different solution groups. These results suggest that the quantity of fructose reintroduced may have potentially been too small to elicit symptomatic responses or that IBS participants in this study who respond to a LFD have a fructose tolerance above the largest quantity tested, 15 g.
Conclusions There were no IBS symptom differences in the fructose or fructose in excess of glucose compared to glucose alone in participants with non-constipated IBS who responded to an LFD. Fructose may be tolerated at higher quantities than those typically assessed in the reintroduction phase in IBS patients who respond to an LFD. Future studies should investigate symptomatic responses to higher quantities of fructose in both the fructose alone and fructose excess groups. Optimal symptom assessment endpoints and duration of FODMAP reintroduction needs to be studied.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/93529227931?pwd=UzZINVEreXNaTHBpUDdJclUxTHVPUT09 Password: 051963