-
Author
Emily Nguyen -
PI
Ilina Pluym M.D.
-
Co-Author
Daniel Lee MD, Ilina Pluym MD
-
Title
Maternal outcomes and disparities after labor induction in a tertiary health care center
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
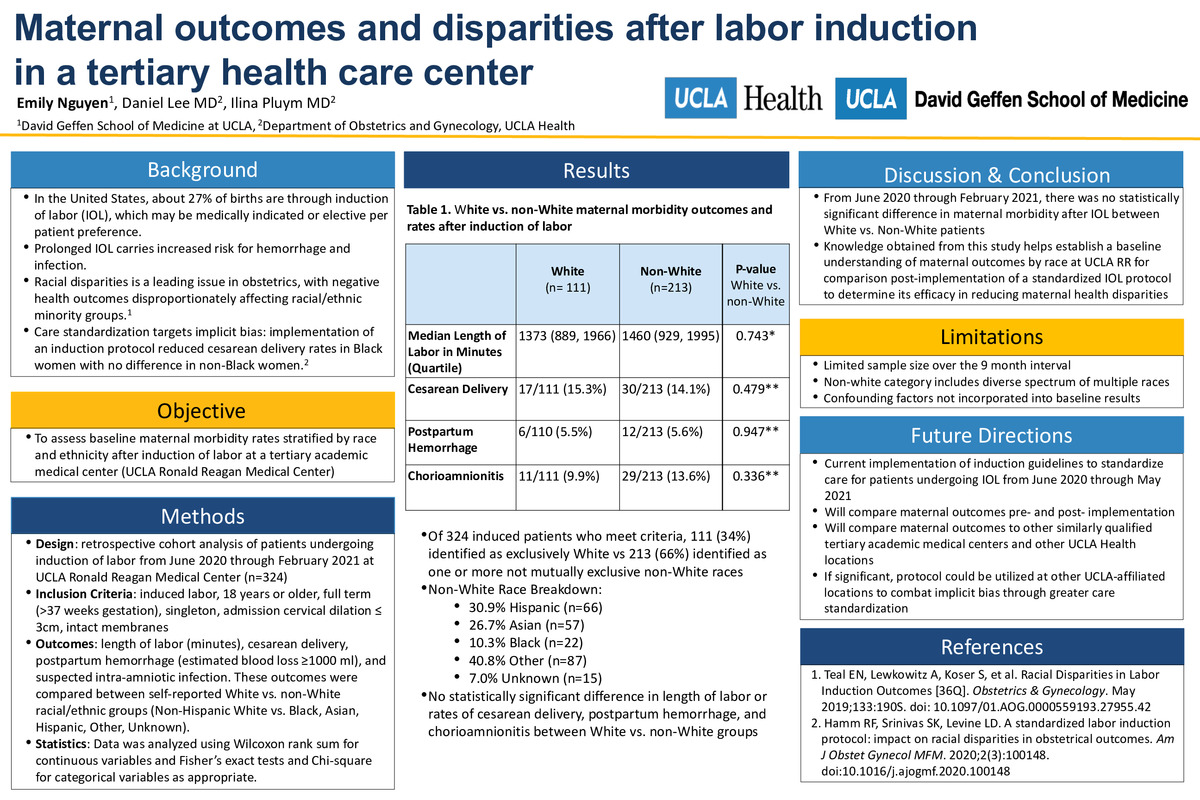
Background: Racial disparities is a leading issue in obstetrics in the United States, with morbid outcomes disproportionately affecting racial and ethnic minorities. In the United States, approximately 27% of births are through induction of labor (IOL), which may be medically indicated or elective per patient preference. Shortening the time to delivery during induction of labor is important to decrease maternal complications of hemorrhage and infection. While causes of racial disparities in health care are multifactorial, care standardization has been shown to reduce health inequities by targeting implicit biases.
Objective: To assess baseline maternal morbidity rates after induction of labor by race and ethnicity at a tertiary academic medical center.
Study Design: A retrospective cohort analysis was completed of patients undergoing IOL from June 2020 through February 2021 at UCLA Ronald Reagan Medical Center (UCLA RR). Patients undergoing induction were included if they were >18 years old, singleton, full term, with intact membranes, and had an admission cervical dilation ≤ 3cm (n=324). Outcomes included length of labor, cesarean delivery, postpartum hemorrhage (estimated blood loss ≥ 1000 ml), and chorioamnionitis among White vs. non-White racial/ethnic groups (Non-Hispanic White vs. Black, Asian, Hispanic, Other). Data was analyzed using Wilcoxon rank sum for continuous variables and Fisher’s exact tests and Chi-square for categorical variables as appropriate.
Results: There were 324 patients admitted for IOL among which 111 (34%) identified as exclusively White vs 213 (66%) that identified as one or more not mutually exclusive non-White races (30.9% Hispanic, 26.7% Asian, 10.3% Black, 40.8% Other and 7.0% Unknown). The average length of labor for White patients was 1373 minutes compared to 1460 minutes for non-White patients. Among White vs non-White patients, there was no difference in rates of cesarean section (15.3% vs 14.1%, p=0.479), postpartum hemorrhage (5.5% vs 5.6%, p=0.957) or chorioamnionitis (9.9% vs 13.6%, p=0.336).
Conclusion: Although there was no statistical difference in maternal morbidity between White vs. non-White mothers, limited by small sample size, knowledge obtained from this study will establish a baseline understanding of maternal IOL outcomes at UCLA RR to target in a standardized protocol for induction. This retrospective cohort analysis is part of a larger quality improvement project that aims to take steps toward mitigating racial disparities in the UCLA Health System through care standardization. -
PDF
-
Zoom
https://uclahs.zoom.us/j/91328493879?pwd=ZW9CcUJldUE0OVhhZWRmQTBUa2Jrdz09