-
Author
Gurjit Kaur -
PI
Amy Shekarchi, MD
-
Co-Author
-
Title
Patient’s Primary Care Utilization After Social Needs Screening
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
Title and Author: Patients’ Primary Care Utilization After Social Needs Screening by Gurjit Kaur, MS2 (Charles R. Drew University of Medicine and Science/David Geffen School Of Medicine at UCLA, Amy Shekarchi, MD: Pediatrics - Olive View UCLA
Objective: The purpose of the current study is to investigate the primary care utilization of patients three years after social needs screening.
Importance: Unmet social needs are linked to poorer health outcomes in children and increased prevalence of chronic diseases. Even though the exact mechanism linking unmet social needs and health status is not clear, population studies suggest that unmet social needs are contributing to increased mortality risk in the United States. Primary care is a way patients can receive support for unmet social needs. Access to and utilization of primary care improves health outcomes. Given the impact of unmet social needs on health status, investigating the role of primary care utilization in patients screened for social needs can be a starting point to explore screening effectiveness, barriers, and facilitators in the primary care setting.
Methods: Parents of 289 pediatric patients ages 0-12 years completed an 11-item social needs screener at an LA County pediatric clinic between October 2017 and May 2019. Each patient’s number of primary care visits attended, missed, and/or cancelled in three years post-screening was retrospectively collected from the patient’s electronic medical record.
289 patients completed the screen. Of those 289 completed screens, 14 were not analyzed due to lack of identifying information and 137 were not analyzed because they had not yet reached 3 years post-screening. Patients’ primary care access data was stratified by whether or not the patient screened positive or negative; and by whether or not the family accepted or declined services if the screen was positive. A positive social needs screen was defined as disclosure of one or more social need. A negative social needs screen was defined as zero disclosed social needs.
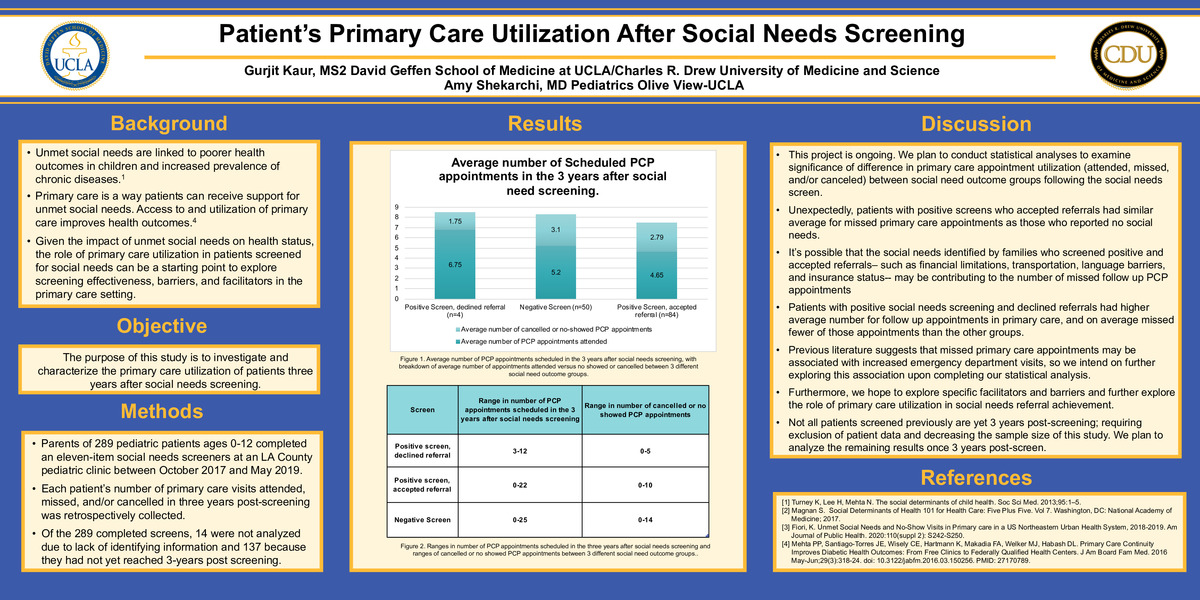
Results: Of the 138 screens analyzed, 50 screens were negative and thus indicated no unmet social needs. 88 total screens were positive and indicated at least one unmet social need. Four of these positive screens declined referral while 84 accepted the referrals. Patients with a positive screen who declined referral had an average number of 8.5 subsequent primary care appointments scheduled after screening (range was 3-12). The average number of primary care visits that these patients cancelled or did not show for was 1.75 (range of 0-5).
The average number of primary care appointments scheduled after screening for patients with a negative screen was 8.3 (range of 0-25). The average number of primary care appointments that patients with a negative screen cancelled or no showed to was 3.1 (range of 0-14). The average number of follow up primary care appointments scheduled after screening for patients with a positive screen who accepted referrals was 7.4 (range of 0-22). The average number of primary care appointments with cancellation or no show for patients with a positive screen who accepted referrals was 2.8 (range of 0-10).
Discussion:
This project is ongoing. We plan to conduct statistical analyses to examine significance of difference in primary care appointment utilization (attended, missed, and/or canceled) between social need outcome groups following the social needs screen. Unexpectedly, patients with positive screens who accepted referrals had a similar average for missed primary care appointments as those who reported no social needs. It is possible that the social needs identified by families who screened positive and accepted referrals– such as financial limitations, transportation, language barriers, and insurance status-- may be contributing to the number of missed follow-up primary care appointments. Patients with positive social needs screening and declined referrals had higher average number for follow up appointments in primary care, and on average missed fewer of those appointments than the other groups. Previous literature suggests that missed primary care appointments may be associated with increased emergency department visits, so we intend on further exploring this association upon completing our statistical analysis. Not all patients screened previously are yet 3 years post-screening; requiring exclusion of patient data and decreasing the sample size of this study.
Future Direction:
This project is ongoing, and we plan to conduct statistical analyses to examine significance associations between missed appointments during the first year following the social needs screen and social screen outcomes. We plan to analyze the remaining results once 3 years post-screen in order to include all of the screens that were conducted.
We plan to gain additional insight on the relationship between primary care utilization and the different social needs outcome groups. We hope this can help us ultimately explore specific barriers and facilitators to achievement of social needs referrals. We are considering conducting patient interviews to collect qualitative data about such facilitators and barriers and further explore the role of primary care utilization in social needs referral achievement.
References
[1] Turney K, Lee H, Mehta N. The social determinants of child health. Soc Sci Med. 2013;95:1–5.
[2] Magnan S. Social Determinants of Health 101 for Health Care: Five Plus Five. Vol 7. Washington, DC: National Academy of Medicine; 2017.
[3] Fiori, K. Unmet Social Needs and No-Show Visits in Primary care in a US Northeastern Urban Health System, 2018-2019. Am Journal of Public Health. 2020:110(suppl 2): S242-S250.
[4] Mehta PP, Santiago-Torres JE, Wisely CE, Hartmann K, Makadia FA, Welker MJ, Habash DL. Primary Care Continuity Improves Diabetic Health Outcomes: From Free Clinics to Federally Qualified Health Centers. J Am Board Fam Med. 2016 May-Jun;29(3):318-24. doi: 10.3122/jabfm.2016.03.150256. PMID: 27170789.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/92979548534?pwd=RTlpbGFmblFoSGJRcTlGeldBUm4xQT09