-
Author
Spencer Flynn -
PI
Tamara Horwich, MD, MS
-
Co-Author
Preethi Srikanthan, MD; Kosuke Inoue, MD; Karol Watson, MD, PhD
-
Title
Urinary Stress Hormones and Cardiovascular Events in Pre- and Post-Menopausal Women vs. Men: The Multi-Ethnic Study of Atherosclerosis
-
Program
Internal Medicine Chief's Fellowship
-
Other Program (if not listed above)
-
Abstract
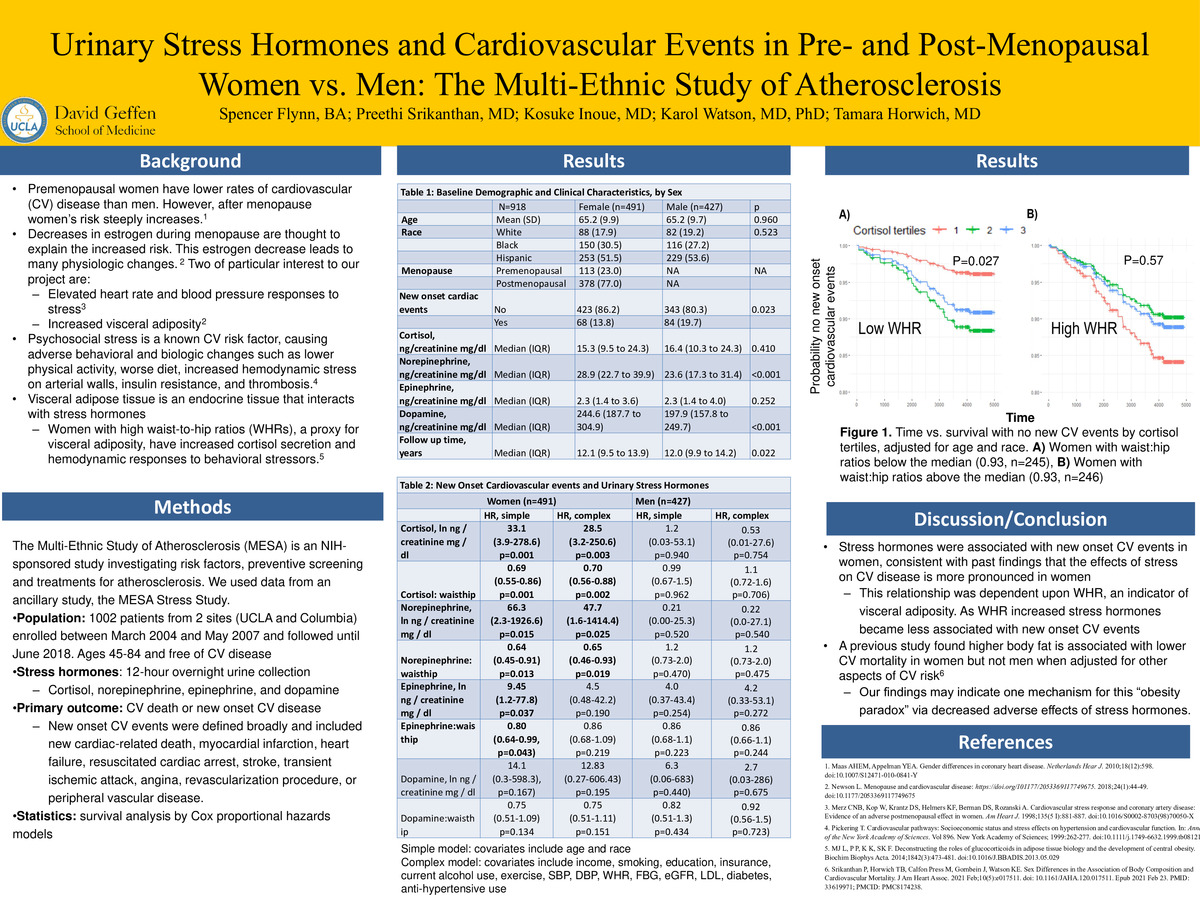
Background: Women experience an increased risk of cardiovascular (CV) disease after menopause. Menopause has been linked to various CV changes and risk factors. Two of these are increased responses to stress including elevated heart rate and blood pressure responses as well increased visceral adiposity. Visceral adipose tissue is an endocrine tissue that may interact with the stress response and stress hormones such as cortisol, epinephrine, norepinephrine, and dopamine. For example, women with high waist-to-hip ratios (WHRs), a proxy for visceral adiposity, have increased cortisol secretion and hemodynamic responses to behavioral stressors.
Methods: There were 1002 patients enrolled in the Multi-ethnic Study of Atherosclerosis (MESA) Stress I Study. Patients were enrolled from 2 sites (UCLA and Columbia) between March 2004 and May 2007 and followed until June 2018. Patients were ages 45-84 and free of CV disease. Stress hormones (cortisol, norepinephrine, epinephrine, and dopamine) were quantified by 12-hour overnight urine collection. Visceral adiposity was quantified as WHR. The primary outcome was new onset CV disease or CV death. Risk of new onset CV disease was determined through Cox proportional hazards models. All Cox models included each individual stress hormone levels and WHR as predictor variables, as well as an interaction term between stress hormones and WHR . A simple model included age and race as covariates. A complex model was adjusted for 14 additional prespecified covariates associated with CV risk.
Results: There were 918 total patients with complete demographic and clinical data, consisting of 491 women and 427 men. For the simple model, cortisol, norepinephrine, and epinephrine were all associated with increased risk of new onset CV events in women but not in men (HR 33.1 (3.9-278.6), 66.3 (2.3-1926.6), and 9.45 (1.2-77.8), respectively; all P<0.05). In the complex models, cortisol and norepinephrine were associated with new onset CV events in women but not men (HR 28.5 (3.2-250.6), P=0.003; and HR 47.7 (1.6 -1414.4), P=0.025). Interaction terms consistently indicated that as WHR increased the association between stress hormones (cortisol, norepinephrine, and epinephrine) and new onset CV events decreased (HR varied between 0.6-0.7, all P<0.05).
Conclusion: Cortisol, epinephrine, and norepinephrine were associated with CV outcomes in women but not men in this cohort. This is consistent with previous findings that effects of stress on CV disease is more pronounced in women. This relationship was dependent upon WHR, which is an indicator of visceral adiposity. As WHR increased, cortisol, norepinephrine, and epinephrine became less associated with new CV events. This finding may indicate that increased WHR confers some measure of resistance to the CV effects of stress hormones.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/93841414821?pwd=V3AwRm9rUU56UW53VEV6b2gxOXZyUT09