-
Author
Stephanie Hernandez -
PI
Joseph DiNorcia, MD
-
Co-Author
Paul Hsu, MPH, PhD
-
Title
Emergency Room Visits and Hospital Readmissions During the Pandemic: How COVID-19 Changed Outpatient Care of Liver Transplant Recipients at UCLA
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
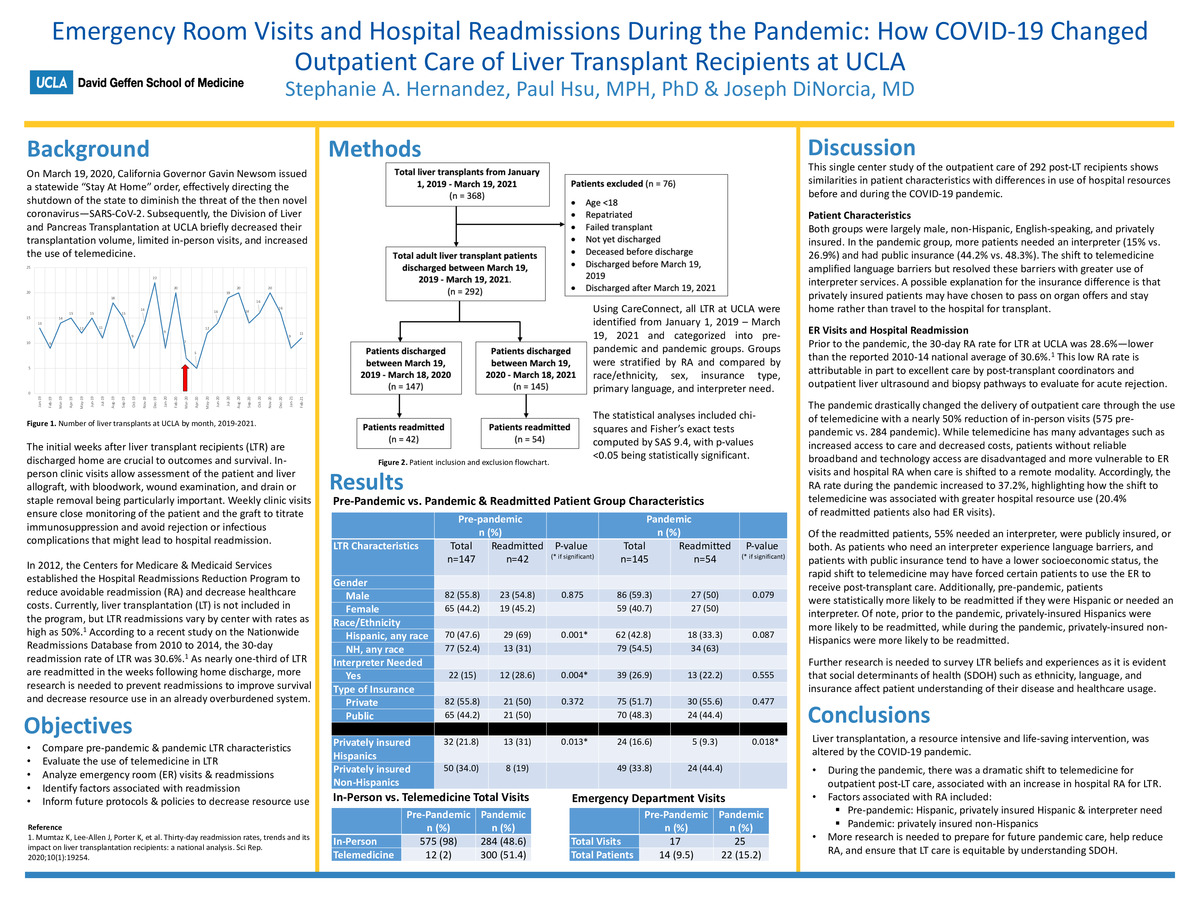
Background:
The COVID-19 pandemic altered the field of organ transplantation resulting in decreases in referrals, waitlist additions, and transplant volumes along with the implementation of telemedicine of which the effects to recipients and their outcomes including ER visits and hospital readmissions (RA) are largely unknown. According to a recent study on the Nationwide Readmissions Database from 2010 to 2014, the 30-day readmission rate of liver transplant recipients (LTR) was 30.6%. As nearly one-third of LTR are readmitted in the weeks following home discharge, more research is needed to prevent readmissions to improve survival and decrease the burden on healthcare, especially in an already overburdened state. This study aims to compare pre-pandemic & pandemic LTR characteristics, analyze the frequency of emergency room visits and readmissions while identifying factors that can inform future protocols and policies to decrease avoidable resource utilization.Methods:
Using CareConnect, all liver transplant recipients at UCLA Medical Center were identified from January 1, 2019 – March 19, 2021, and further categorized into pre-pandemic (March 19, 2019-March 18, 2020) and pandemic groups (March 19, 2020 – March 18, 2021). Groups were stratified by RA and compared by race/ethnicity, sex, insurance type, primary language, and interpreter need. The statistical analyses included chi-squares and Fisher’s exact tests computed by SAS 9.4, with p-values <0.05 being statistically significant.Results:
This single center study on the outpatient care of 292 post-liver transplant recipients showed similarities in patient characteristics with differences in use of hospital resources before and during the COVID-19 pandemic. Both groups were largely male, non-Hispanic, English-speaking, and privately insured. In the pandemic group, more patients needed an interpreter (15% vs. 26.9%) and had public insurance (44.2% vs. 48.3%). Prior to the pandemic, the 30-day RA rate for LTR at UCLA was 28.6%—lower than the reported 2010-14 national average of 30.6%. The pandemic drastically changed the delivery of outpatient care through the use of telemedicine with a nearly 50% reduction of in-person visits (575 pre-pandemic vs. 284 pandemic). The RA rate during the pandemic increased to 37.2% and 20.4% of readmitted patients also had ER visits. Of the readmitted patients, 55% needed an interpreter, were publicly insured, or both.Additionally, pre-pandemic patients were statistically more likely to be readmitted if they were Hispanic or needed an interpreter. Of note, prior to the pandemic, privately-insured Hispanics were more likely to be readmitted, while during the pandemic, privately-insured non-Hispanics were more likely to be readmitted.
Conclusions:
Liver transplantation, a resource intensive and life-saving intervention associated with increases in survival, was altered by the COVID-19 pandemic. In this analysis of emergency room visits and hospital readmissions before and after the pandemic, there was an increase in LTR resource utilization. The RA rate for LTR at UCLA increased dramatically during the pandemic (37.2% vs. 28.6%). The low pre-pandemic RA rate is attributable in part to excellent post-transplant coordinator care and outpatient ultrasound and biopsy pathways to evaluate for acute rejection. Additionally, during the pandemic, 20.4% of LTRs who visited the ER but were not admitted ultimately were readmitted at another time. Pre-pandemic factors associated with RA were Hispanic ethnicity, interpreter need, and privately insured Hispanic subgroups while factors associated with RA during the pandemic included privately insured non-Hispanics. As patients who need an interpreter experience language barriers and patients with public insurance tend to have a lower socioeconomic status, the rapid shift to telemedicine may have forced certain patients to use the ER to receive post-transplant care. More research is needed to prepare for future crises and inform interventions and policies to prevent avoidable LTR resource utilization and make LT more equitable by understanding social determinants of care such as ethnicity, language, and insurance type that affect patient beliefs and healthcare usage. -
PDF
-
Zoom
https://uclahs.zoom.us/j/99569070165?pwd=STA3K0NCMDdLWS9CWEh5NFhHdGljUT09