-
Author
Vartan Matossian -
PI
Jeffrey L. Saver
-
Co-Author
Vartan Matossian
-
Title
Additional Brain Ischemia Protection Time with Prehospital Versus In-Hospital Neuroprotective Agent Start
-
Program
Medical Student Training in Aging (MSTAR) Research Program
-
Other Program (if not listed above)
-
Abstract
Title: Additional Brain Ischemia Protection Time with Prehospital Versus In-Hospital Neuroprotective Agent Start
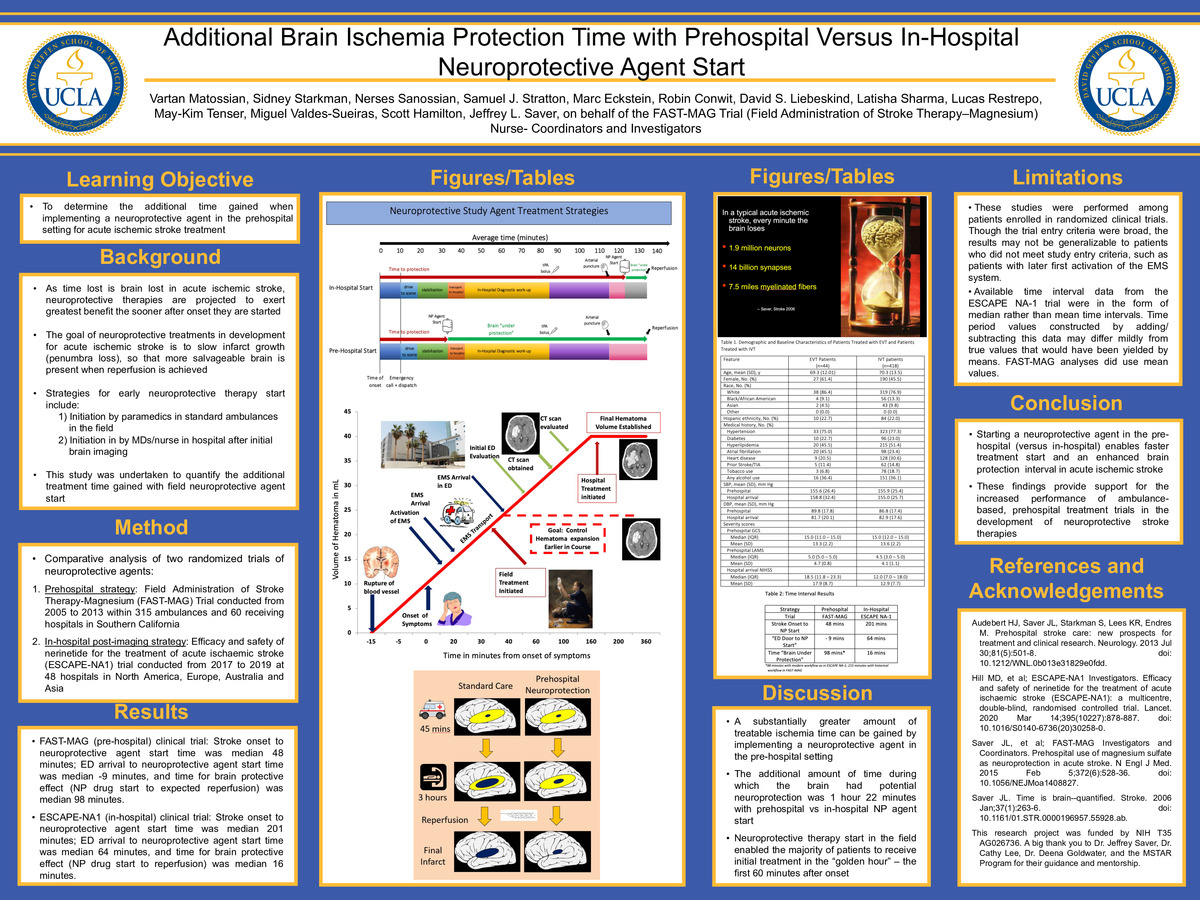
Importance: As time lost is brain lost in acute ischemic stroke, neuroprotective therapies are projected to exert greatest benefit the sooner after onset they are started. The goal of neuroprotective treatments in development for acute ischemic stroke is to slow infarct growth (penumbra loss), so that a more salvageable brain is present when reperfusion is achieved. This study was undertaken to quantify the additional treatment time gained with field neuroprotective agent start.
Objective: To determine the additional time gained when implementing a neuroprotective agent in the prehospital setting for acute ischemic stroke treatment.
Design, Settings, and Participants: Comparative analysis of two randomized trials of neuroprotective agents: 1) the prehospital strategy Field Administration of Stroke Therapy-Magnesium (FAST-MAG) Trial conducted from 2005 to 2013 within 315 ambulances and 60 receiving hospitals in Southern California; 2) the in-hospital post initial imaging strategy Efficacy and safety of nerinetide for the treatment of acute ischaemic stroke (ESCAPE-NA1) trial conducted from 2017 to 2019 at 48 hospitals in North America, Europe, Australia and Asia.
Main Outcomes and Measures: The main outcomes were median time measurements in the treatment of acute ischemic stroke: minutes from stroke onset to neuroprotective drug start, minutes from emergency department arrival to neuroprotective drug start, and minutes for “brain under protection”, defined as neuroprotective drug start to expected/actual reperfusion.
Results: FAST-MAG (pre-hospital) clinical trial: Stroke onset to neuroprotective agent start time was median 48 minutes; ED arrival to neuroprotective agent start time was median -9 minutes, and time for brain protective effect (NP drug start to expected reperfusion) was median 98 minutes. ESCAPE-NA1 (in-hospital) clinical trial: Stroke onset to neuroprotective agent start time was median 201 minutes; ED arrival to neuroprotective agent start time was median 64 minutes, and time for brain protective effect (NP drug start to reperfusion) was median 16 minutes.
Conclusions and Relevance: Starting a neuroprotective agent in the pre-hospital (versus in-hospital) enables faster treatment start and an enhanced brain protection interval in acute ischemic stroke. These findings provide support for the increased performance of ambulance-based, prehospital treatment trials in the development of neuroprotective stroke therapies.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/97870671878?pwd=M3R0Um56dGVtTHEvTERUVzJNRCtSUT09