-
Author
Cheikh Mballo -
PI
Peyman Benharash
-
Co-Author
Zachary Tran
-
Title
Trends and Outcome in the Utilization of Vena Cava Filters: A contemporary study
-
Program
STTP
-
Other Program (if not listed above)
-
Abstract
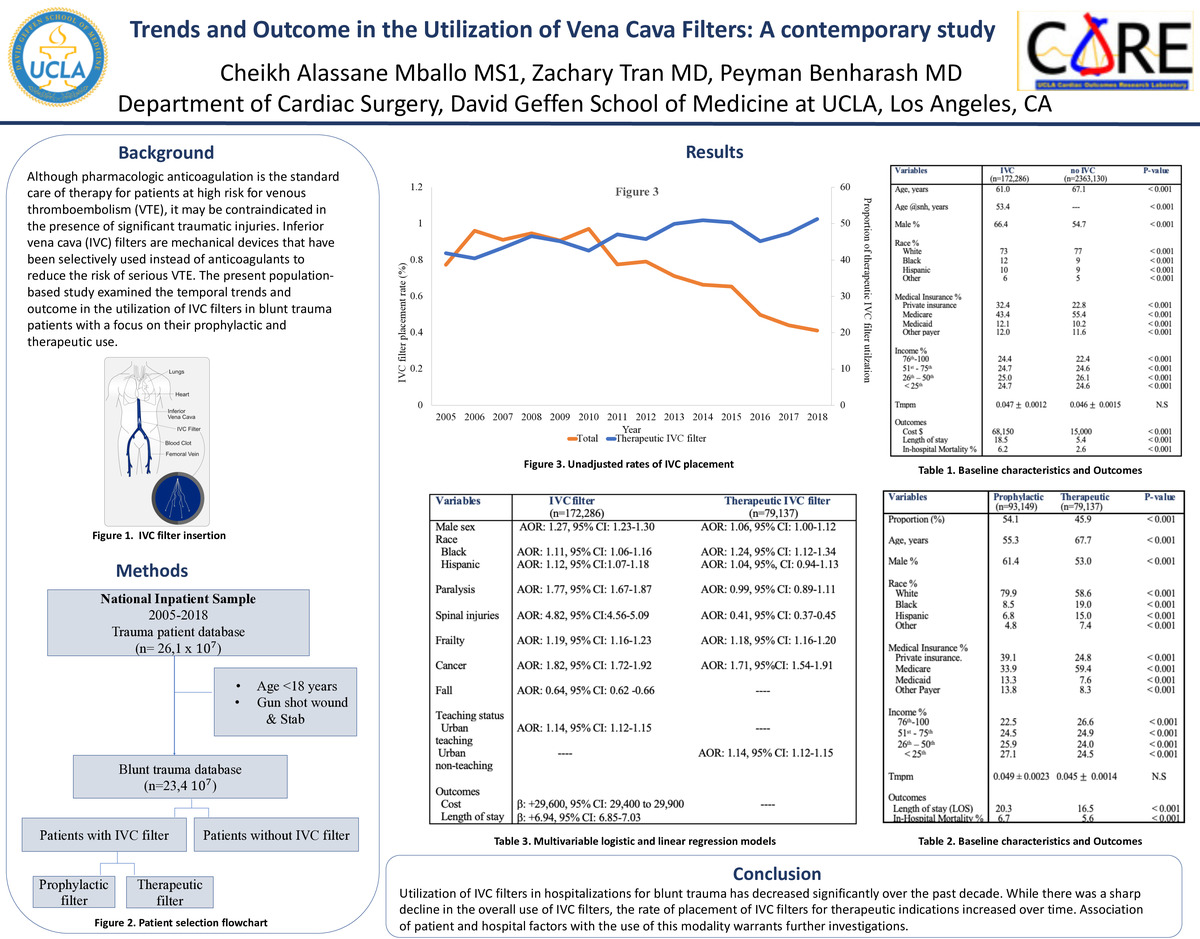
Introduction:
Although pharmacologic anticoagulation is the standard care of therapy for patients at high risk for venous thromboembolism (VTE), it may be contraindicated in the presence of significant traumatic injuries. Inferior vena cava (IVC) filters are mechanical devices that have been selectively used instead of anticoagulants to reduce the risk of serious VTE. The present population-based study examined the temporal trends and outcome in the utilization of IVC filters in blunt trauma patients with a focus on their prophylactic and therapeutic use.
Methods:
The 2005-2018 National Inpatient Sample database was queried to identify all adult patients (≥18 years old) hospitalized for blunt traumatic injuries. The NIS is the largest inpatient database in the United States and is sponsored by the Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP), and provides a sampling of abstracted discharge data representing a 20% stratified sample of all discharged patients from a national survey of all nonfederal acute care hospitals in the United States.
International Classification of Diseases, 9/10th Revision codes, were used to identify all blunt trauma patients who received an IVC filter placement. Filters were defined as therapeutic in the presence of a concomitant diagnostic code for lower extremity VTE and otherwise considered prophylactic. The Trauma Mortality Prediction Model (tmpm score, scale 0-1 with 1 predicting mortality) was used to evaluate the severity of injuries. Temporal trends in IVC filter placement were examined using non-parametric tests for trend (np-trend). Multivariable regression models were developed to assess outcomes and factors independently associated with the use of IVC filters.
Results:
Of an estimated 23,354,169 blunt trauma patients meeting inclusion criteria, 172,286 (0.74%) underwent an IVC filter placement. The proportion of patients receiving an IVC filter decreased significantly from 0.77% in 2005 to 0.44% in 2018 (p-trend<0.001) following a peak in 2010. Blunt trauma patients who received IVC filters were on average younger (61.0 vs 67.1 years old), more likely to be of either Black or Hispanic races (12 vs 9% vs 10 vs 9%, respectively), insured by private insurance (32.4 vs 22.8%), and treated in the South (41.0 vs 38.2%, p<0.001). In addition, compared to those who did not undergo an IVC filter placement, blunt trauma patients who received an IVC filter had a longer average hospital length of stay (18.5 vs 5.4 days, p<0.001) and higher cost burden ($68,140 vs $15,000, p<0.001). On adjusted analysis, factors associated with increased odds of receiving an IVC filter included male sex (AOR: 1.27, 95% CI: 1.23-1.30), Black and Hispanic races (AOR:1.11, 95% CI: 1.06-1.16 & AOR:1.12, 95% CI:1.07-1.18, respectively), paralysis (AOR: 1.77, 95% CI: 1.67-1.87), cancer (AOR: 1.82, 95% CI: 1.72-1.92) and treatment at an urban teaching hospital (AOR: 1.73, 95% CI:1.60-1.88, reference: rural non-teaching hospital). Furthermore, IVC filter placement was associated with increased cost (b: +29,600, 95% CI: 29,400 to 29,900) and length of stay (b: +6.94, 95% CI: 6.85-7.03).
Following stratification of the type of IVC filter by indication, we found that of the overall IVC filters used, 45.9% were placed for therapeutic indication. Prophylactic filter placement was more commonly covered by private insurance (39.1% vs 24.8%, p<0.001) while placement of a therapeutic filter was more commonly covered by Medicare insurance (59.4% vs 33.9%, p<0.001). Compared with patients who received a prophylactic filter, patients with a therapeutic IVC filter had lower unadjusted rates of in-hospital mortality (6.7% vs 5.6%, p<0.001) and had a shorter length of stay (20.3 vs 16.5 days, p<0.001). After adjustment, factors associated with increased odds of receiving therapeutic filters included male sex (AOR: 1.06, 95% CI: 1.00-1.12), black race (AOR: 1.24, 95% CI: 1.12-1.34) and treatment at an urban non-teaching hospital (AOR: 1.14, 95% CI: 1.12-1.15). Furthermore frailty (AOR: 1.18, 95% CI: 1.11-1.26) and cancer (AOR: 1.68, 95% CI: 1.51-1.88) were associated with increased odds of receiving therapeutic IVC filter placement, while spinal injuries (AOR: 0.43, 95% CI: 0.38-0.48) were not. There were no significant differences in the Trauma Injury Scores of those receiving IVC filters for therapeutic (TMPM score: 0.045 ± 0.0014) compared with prophylactic (0.049 ± 0.0023) indications.
Conclusion:
Utilization of IVC filters in hospitalizations for blunt trauma has decreased significantly over the past decade. While there was a sharp decline in the overall use of IVC filters, the rate of placement of IVC filters for therapeutic indications increased over time. Association of patient and hospital factors with the use of this modality warrants further investigations.
-
PDF
-
Zoom