-
Author
Emily Lin -
Co-author
Shirley Jiang, MD, Zekun Feng, MD, Ed Ha, MD
-
Title
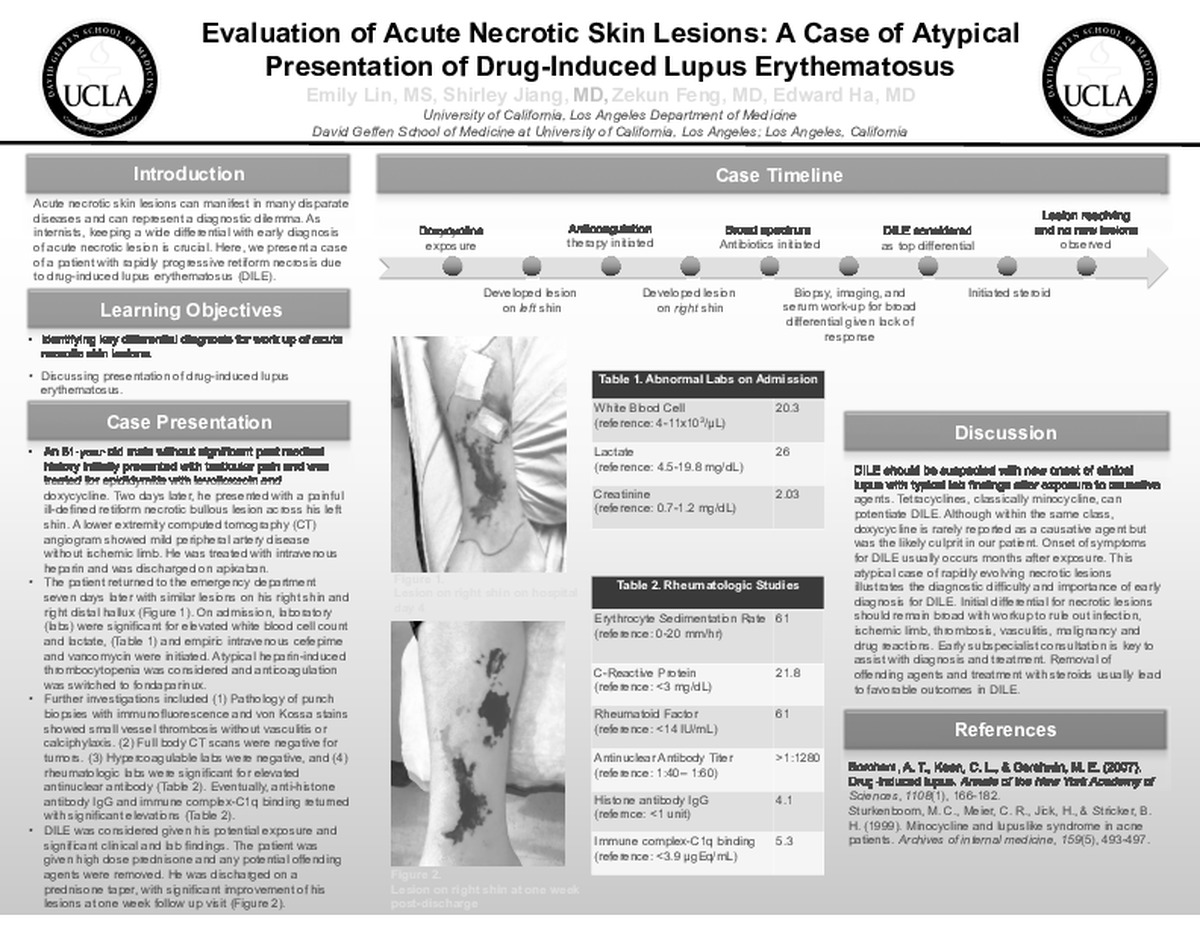
Evaluation of Acute Necrotic Skin Lesions: A Case of Atypical Presentation of Drug-Induced Lupus Erythematosus
-
Abstract
Introduction:
Acute necrotic skin lesions can manifest in many disparate diseases and can represent a diagnostic dilemma. Therefore, keeping a wide differential with early diagnosis of acute necrotic lesion is crucial. Here, we present a case of a patient with rapidly progressive retiform necrosis due to drug-induced lupus erythematosus (DILE).
Case Description:An 81-year-old man with coronary artery disease and without previous rheumatologic disorder was treated for epididymitis with levofloxacin and doxycycline. Two days later, he presented to outside hospital with a painful ill-defined retiform necrotic bullous lesion with peripheral erythema across his left shin. Lower extremity CT angiogram ruled out ischemic limb but showed mild peripheral artery disease, thus he was treated with intravenous heparin and was discharged on apixaban. Seven days later, he developed similar lesions on his right shin and right distal hallux and returned to the ED. Laboratory findings showed leukocytosis of 20,280/μL, elevated lactate of 26 mg/dL, platelet of 217×109/L and creatinine of 2.03 mg/dL. Intravenous cefepime and vancomycin were initiated for possible infection. Further evaluations for hypercoagulable and rheumatologic etiologies were only significant for elevated antinuclear antibody titer of >1:1280, with negative biomarkers including ANCA, anti-double stranded DNA, anti-Smith, anti-RNP, DRVVT, cardiolipin ab, and beta-2-glycoprotein. Punch biopsies with immunofluorescence and von Kossa stains showed small vessel thrombosis without vasculitis or calciphylaxis. Given concerns for atypical heparin-induced thrombocytopenia, heparin was switched to fondaparinux. Full body CT scans were negative for obvious tumors. Unfortunately, the lesions continued to expand with new lesions now developing on his left lower extremity. Eventually, anti-histone antibody IgG resulted at 4.1 units (negative: <1 unit), with elevated immune complex-C1q binding at 5.3 μgEq/mL (normal: <3.9 μgEq/mL). DILE was considered given his potential exposure and corroborating clinical and lab findings. The patient was treated with high dose prednisone and removal of any potential offending agents. His lesions improved and he was discharged on a prednisone taper.
Discussion:
DILE should be suspected with new onset of clinical lupus with typical lab findings after exposure to causative agents. Tetracyclines, classically minocycline, can potentiate DILE. Although within the same class, doxycycline is rarely reported as a causative agent but was the likely culprit in our patient. Onset of symptoms for DILE usually occurs months after exposure. This atypical case of rapidly evolving necrotic lesions illustrates the diagnostic difficulty and importance of early diagnosis for DILE. Initial differential for necrotic lesions should remain broad with workup to rule out infection, ischemic limb, thrombosis, vasculitis, malignancy and drug reactions. Early subspecialist consultation is key to assist with diagnosis and treatment. Removal of offending agents and treatment with steroids usually lead to favorable outcomes in DILE.
-
College
PCC
-
Zoom
https://us02web.zoom.us/j/81775450774?pwd=dHpIRlc2YnNOM3FQVks1ajROajNkdz09
-
PDF