-
Author
Abhinav Sharma -
Co-author
Jonathan Vigdorchik, M.D.
-
Title
A Simple Hip-Spine Classification for Total Hip Replacement – Validation and Large Multi-Center Series
-
Abstract
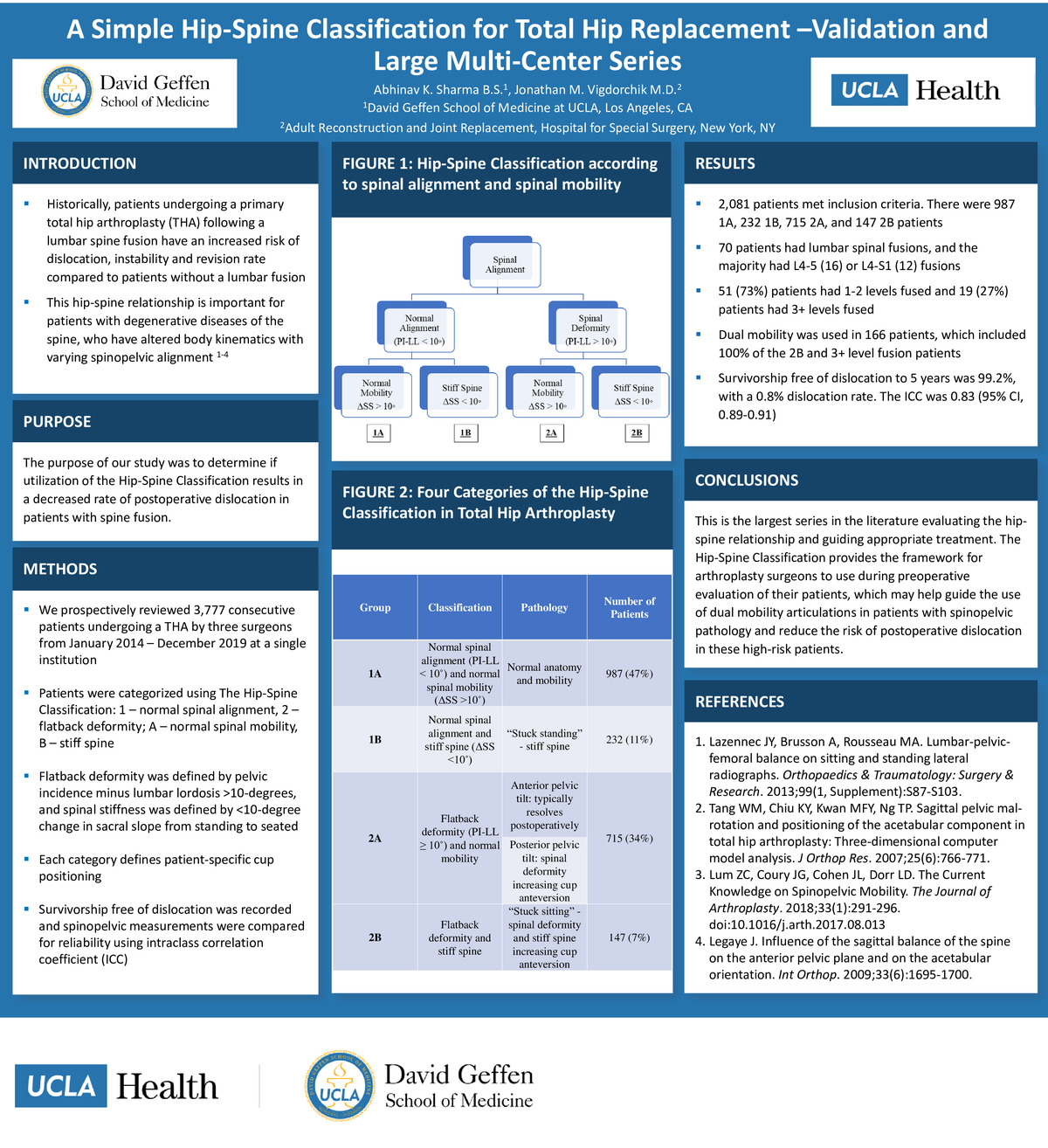
Background: Patients undergoing primary total hip arthroplasty (THA) following a lumbar spine fusion have an increased risk of dislocation and revision compared to those without fusion. The purpose of our study was to determine if utilization of the Hip-Spine Classification results in a decreased rate of postoperative dislocation in patients with spine fusion. Methods: This prospective multi-center study evaluated 3,777 consecutive patients undergoing THA by three surgeons from January 2014 to December 2019. Patients were categorized using The Hip-Spine Classification: 1 – normal spinal alignment, 2 – flatback deformity; A – normal spinal mobility, B – stiff spine. Flatback deformity was defined by pelvic incidence minus lumbar lordosis >10-degrees, and spinal stiffness was defined by <10-degree change in sacral slope from standing to seated. Each category defines patient-specific cup positioning. Survivorship free of dislocation was recorded and spinopelvic measurements were compared for reliability using intraclass correlation coefficient (ICC). Results: 2,081 patients met inclusion criteria. There were 987 1A, 232 1B, 715 2A, and 147 2B patients. 70 patients had lumbar spinal fusions, and the majority had L4-5 (16) or L4-S1 (12) fusions. 51 (73%) patients had 1-2 levels fused and 19 (27%) patients had 3+ levels fused. Dual mobility was used in 166 patients, which included 100% of the 2B and 3+ level fusion patients. Survivorship free of dislocation to 5 years was 99.2%, with a 0.8% dislocation rate. The ICC was 0.83 (95% CI, 0.89-0.91). Conclusion: This is the largest series in the literature evaluating the hip-spine relationship and guiding appropriate treatment. The Hip-Spine Classification provides the framework for arthroplasty surgeons to use during preoperative evaluation of their patients, which may help guide the use of dual mobility articulations in patients with spinopelvic pathology and reduce the risk of postoperative dislocation in these high risk patients.
-
College
AAC
-
Zoom
https://us04web.zoom.us/j/8250839618?pwd=TDR6cTVucUs1L0lSa2RYb3NPTGlOdz09
-
PDF