-
Author
Robera Oljira -
Co-author
Robera Oljira, Brannen Liang M.D.
-
Title
TEMPI Syndrome: Disease Progression and Response to Treatment
-
Abstract
Introduction
TEMPI syndrome, characterized by telangiectasias, erythrocytosis and elevated erythropoietin, monoclonal gammopathy, perinephric fluids collections, and intrapulmonary shunting was only recently described in 2011. To our knowledge, there are fewer than 15 reported cases worldwide. This case report explores the complex pathophysiology and serves to raise awareness for this rare disease.
Case Presentation
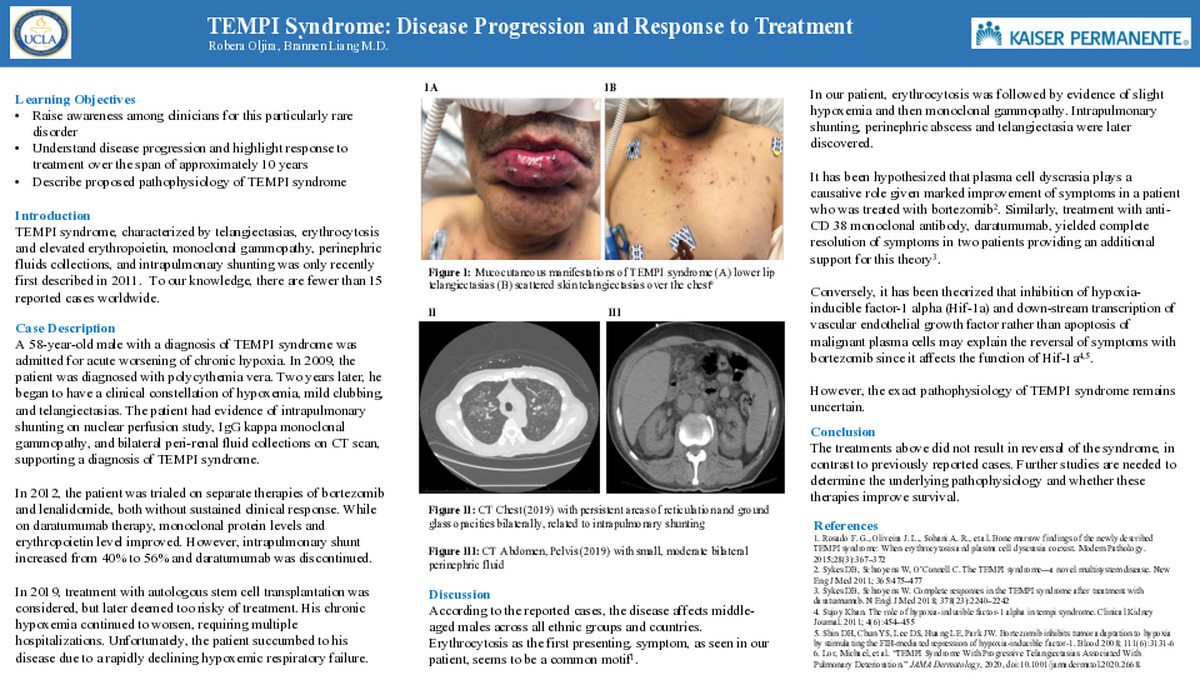
A 58-year-old male with a diagnosis of TEMPI syndrome was admitted for acute worsening of chronic hypoxia. Two years prior to his diagnosis, the patient was initially diagnosed with polycythemia vera. In 2011, he began to have a clinical constellation of hypoxemia, mild clubbing, and telangiectasias. The patient also had evidence of intrapulmonary shunting on nuclear perfusion study, IgG kappa monoclonal gammopathy, and bilateral peri-renal fluid collections on computed tomography scan, supporting a diagnosis of TEMPI syndrome. In 2012, patient was trialed on separate therapies of bortezomib and lenalidomide, both without sustained clinical response. While on daratumumab therapy, monoclonal protein levels and erythropoietin level improved. However, intrapulmonary shunt increased from 40% to 56% and daratumumab was discontinued. In 2019, treatment with autologous stem cell transplantation was considered, but later deemed too risky of treatment. His chronic hypoxemia continued to worsen, requiring multiple hospitalizations. Unfortunately, the patient succumbed to his disease due to a rapidly declining hypoxemic respiratory failure.
Discussion
According to the reported cases, the disease affects middle-aged males across all ethnic groups and countries. Erythrocytosis as the first presenting symptom, as seen in our patient, seems to be a common motif.1 In our patient, erythrocytosis was followed by evidence of slight hypoxemia and then monoclonal gammopathy. Intrapulmonary shunting, perinephric abscess and telangiectasia were later discovered. It has been hypothesized that plasma cell dyscrasia plays a causative role given marked improvement of symptoms in a patient who was treated with bortezomib2. Similarly, treatment with anti-CD 38 monoclonal antibody, daratumumab, yielded complete resolution of symptoms in two patients providing an additional support for this theory3. Conversely, it has been theorized that inhibition of hypoxia-inducible factor-1 alpha (Hif-1a) and down-stream transcription of vascular endothelial growth factor rather than apoptosis of malignant plasma cells may explain the reversal of symptoms with bortezomib since it affects the function of Hif-1a4,5. The exact pathophysiology of TEMPI syndrome remains uncertain.
Conclusion
In our patient, the treatments above did not result in reversal of the syndrome, in contrast to previously reported cases. Further studies are needed to determine the underlying pathophysiology and whether these therapies improve survival.
References
1. Rosado F. G., Oliveira J. L., Sohani A. R., et al. Bone marrow findings of the newly described TEMPI syndrome: When erythrocytosis and plasma cell dyscrasia coexist. Modern Pathology. 2015;28(3):367–372
2. Sykes DB, Schroyens W, O’Connell C. The TEMPI syndrome—a novel multisystem disease. New Eng J Med 2011; 365:475–477
3. Sykes DB, Schroyens W. Complete responses in the TEMPI syndrome after treatment with daratumumab. N Engl J Med 2018; 378(23):2240–2242
4. Sujoy Khan. The role of hypoxia-inducible factor-1 alpha in tempi syndrome. Clinical Kidney Journal. 2011; 4(6):454–455
5. Shin DH, Chun YS, Lee DS, Huang LE, Park JW. Bortezomib inhibits tumor adaptation to hypoxia by stimulating the FIH-mediated repression of hypoxia-inducible factor-1. Blood 2008; 111(6):3131-6
-
College
AAC
-
Zoom
https://us04web.zoom.us/j/71043989039?pwd=bHU5d3JVTlpzeHZpV3djTFREQ3RZZz09
-
PDF