-
Author
Priyanka Naik -
Co-author
Matthew Quirk MD, Yong Seok Lee MD, Steven Raman MD, Michael Douek MD, Simin Bahrami MD, Rinat Masamed MD, Ely Felker MD, Justin McWilliams MD, Vatche Agopian MD, Fady Kaldas MD, Bita Naini MD, David Lu MD
-
Title
Transperitoneal biopsy for cholangiocarcinoma is not associated with increased risk of peritoneal metastasis
-
Abstract
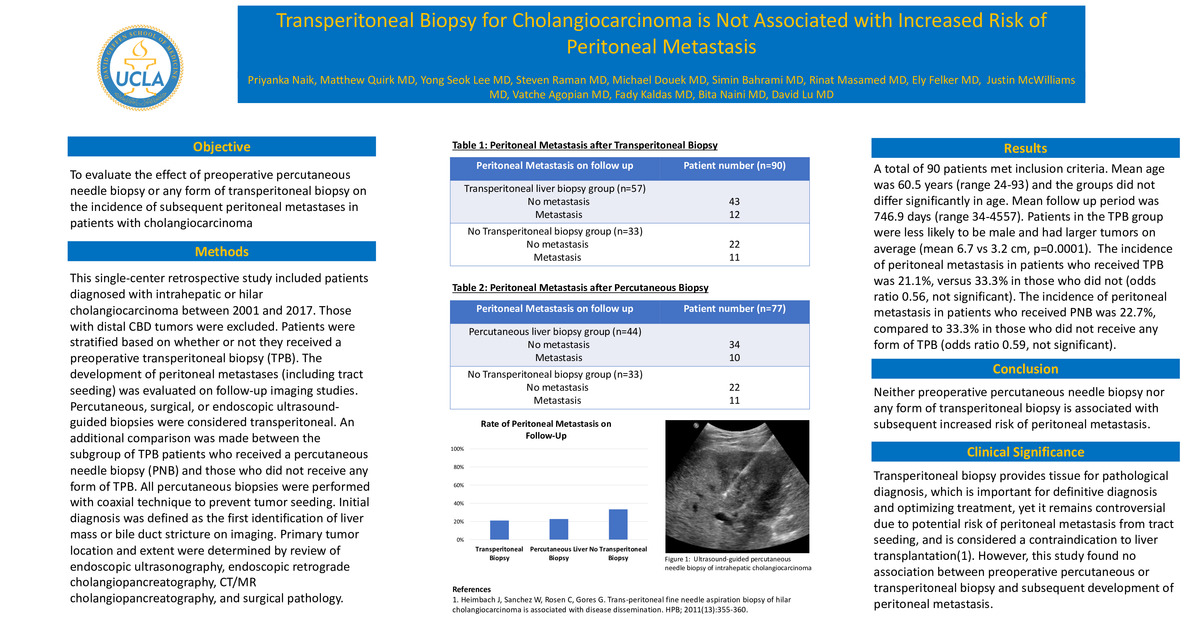
Purpose: To evaluate the effect of percutaneous needle biopsy or any form of transperitoneal biopsy on the incidence of peritoneal metastases in patients with cholangiocarcinoma.
Methods: This single-center retrospective study included patients diagnosed with intrahepatic or hilar cholangiocarcinoma between 2001 and 2017. Those with distal CBD tumors were excluded. Patients were stratified based on whether or not they received a preoperative transperitoneal biopsy (TPB), and the development of peritoneal metastases (including tract seeding) was evaluated on follow-up imaging studies. Percutaneous, surgical, or endoscopic ultrasound-guided biopsies were considered transperitoneal. An additional comparison was made between the subgroup of TPB patients who received a percutaneous needle biopsy (PNB) and those who did not receive any form of TPB. All percutaneous biopsies were performed with coaxial technique to prevent tumor seeding. Initial diagnosis was defined as the first identification of liver mass or bile duct stricture on imaging. Primary tumor location and extent were determined by review of endoscopic ultrasonography, endoscopic retrograde cholangiopancreatography, CT/MR cholangiopancreatography, and surgical pathology.
Results: A total of 90 patients met inclusion criteria. Mean age was 60.5 years (range 24-93) and the groups did not differ significantly in age. Mean follow up period was 746.9 days (range 34-4557). Patients in the TPB group were less likely to be male and had larger tumors on average (mean 6.7 vs 3.2 cm, p=0.0001). The incidence of peritoneal metastasis in patients who received TPB was 21.1%, versus 33.3% in those who did not (odds ratio 0.56, not significant). The incidence of peritoneal metastasis in patients who received PNB was 22.7%, compared to 33.3% in those who did not receive any form of TPB (odds ratio 0.59, not significant).
Conclusion: Neither percutaneous needle biopsy nor any form of transperitoneal biopsy is associated with increased risk of peritoneal metastasis.
Clinical significance: Transperitoneal biopsy provides tissue for pathological diagnosis, which is important for definitive diagnosis and optimizing treatment, yet it remains controversial due to potential risk of peritoneal metastasis and may be considered a contraindication to liver transplantation. This study found no association between preoperative percutaneous or transperitoneal biopsy and subsequent development of peritoneal metastasis.
-
College
PCC
-
Zoom
https://zoom.us/j/97791846846?pwd=NkJzRGh2bG5VM2xkaU5aUGJvcXpLQT09
-
PDF