-
Author
Keara Darragh -
Co-author
Noah Kojima, Marielle Bolano, Andrea Sorensen, Chad Villaflores, Catherine Sarkisian
-
Title
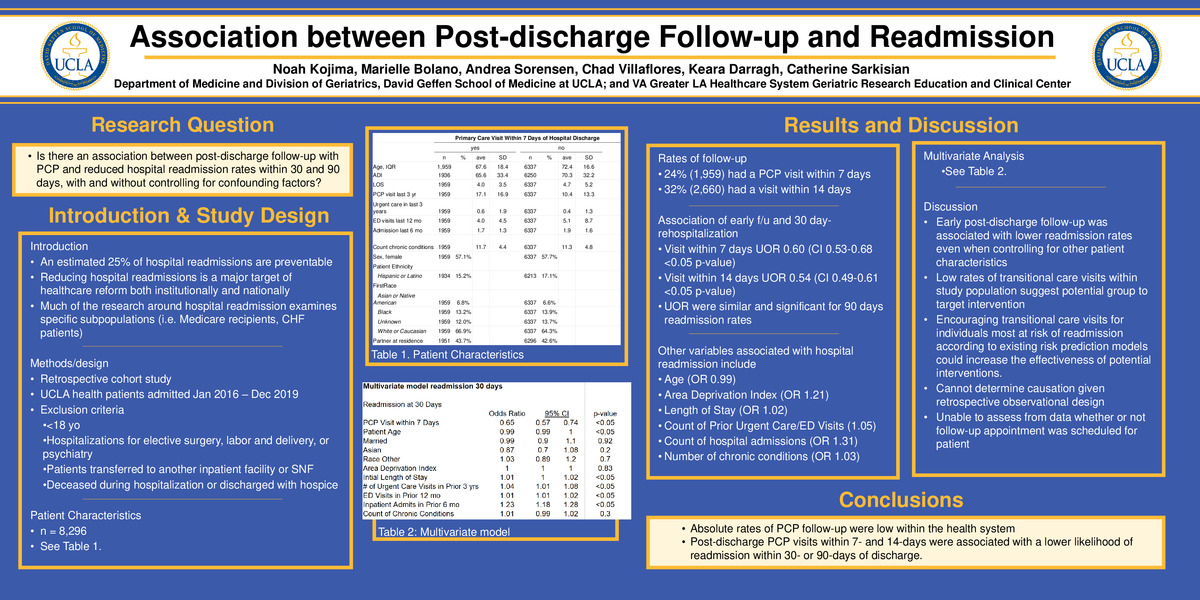
Association between post-hospital follow-up visits with a primary care provider and 30- and 90-day hospital readmissions
-
Abstract
BACKGROUND
Hospital readmissions are a major source of national healthcare expenditures. Many health systems encourage post-hospital primary care provider (PCP) visits, but the literature is mixed as to whether this reduces hospital readmissions. Our study evaluated the association between 7- and 14-day PCP visits and 30- and 90-day hospital readmissions in adult patients within a health system.
METHODS
We performed a retrospective cohort study of patients in a healthcare system located in Los Angeles, CA. Electronic health records of patients hospitalized from January 2016 to November 2019 were evaluated. Adults (age ≥ 18 years) who were discharged home were included. Demographic and clinical characteristics were compiled. Logistic regression models were used to estimate odds ratios (OR) with 95% confidence intervals [95%CI] for readmissions within 30- and 90-days of discharge. The primary predictors were a PCP visit within 7- and 14-days of discharge. In both models we adjusted for sex, age, and number of chronic conditions.
RESULTS
We identified 10,038 patients who met the study inclusion criteria. The median patient age was 70 years (interquartile range: 57, 81);5,806 (57.8%) patients were female, and 8,209 (81.9%) were Caucasian. Overall, 1,922 (18.6%) had a 7-day PCP visit, 2,776 (40.8%) had a 14-day PCP visit, and 7,262 (72.4%) did not see a PCP within 14 days of discharge. The unadjusted OR of readmission for patients with a 7-day PCP visit, versus no 7-day PCP visit, was 0.69, 95%CI: 0.60-0.79, within 30 days of discharge, and 0.67, 95%CI: 0.60-0.76, within 90 days of discharge. The unadjusted OR of hospital readmission for patients with a 14-day PCP visit, versus no 14-day PCP visit, was 0.67, 95%CI: 0.60-0.76, within 30 days of discharge, and 0.70, 95%CI: 0.63-0.77, within 90 days of discharge. The adjusted OR of hospital readmission for patients with a 7-day PCP visit, versus no 7-day PCP visit, was 0.72, 95%CI: 0.63-0.83, within 30 days of discharge, and 0.74, 95%CI: 0.67-0.82, within 90 days of discharge. The adjusted OR of hospital readmission for patients with a 14-day PCP visit, versus no 14-day PCP visit, was 0.70, 95%CI: 0.62-0.79, within 30 days of discharge and 0.76, 95%CI: 0.69-0.83, at 90 days of discharge.
CONCLUSIONS
Most patients in this study did not follow-up with a PCP within 14 days after hospital discharge. Post-discharge PCP visits within 7- and 14-days were associated with a lower likelihood readmission within 30- or 90-days of discharge. Limitations of this study include unmeasured potentially confounding variables such as markers of sickness preventing ability to get to a PCP visit. Despite this limitation, with low rates of PCP visits observed within 7- and 14-days of discharge, a large cohort of patients might benefit from efforts to increase early post-discharge PCP visits. Randomized trials should be conducted to determine whether patient utilization of early post-discharge PCP visits might benefit patients and reduce healthcare expenditure.
-
College
AAC
-
Zoom
https://uclahs.zoom.us/j/98419422947?pwd=SGZuUjRReUFucWNqSVNrcWZWNUhJUT09
-
PDF