-
Author
Jorge Ballon -
Co-author
Adam Kinnaird MD PhD, Rajiv Jayadevan MD, Steve Zhou BS, Danielle E. Barsa BS, Lorna Kwan MPH, Leonard S. Marks MD
-
Title
Magnetic Resonance Imaging Guided Biopsy to Evaluate Prostate Cancer Severity in African American Men
-
Abstract
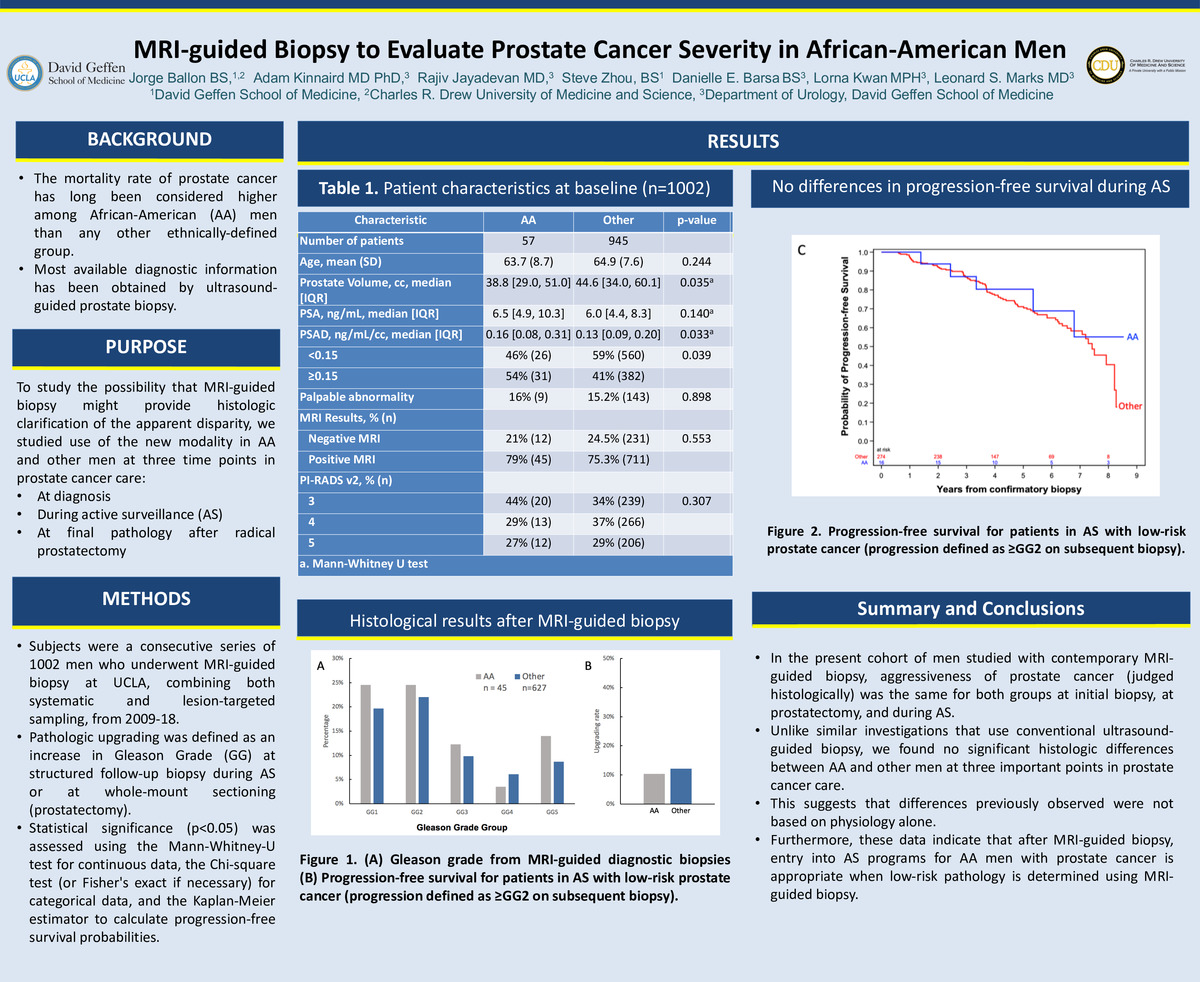
Background: The mortality rate of prostate cancer has long been considered higher among African-American (AA) men. Most diagnostic information has been obtained by ultrasound-guided prostate biopsy.
Objective: To study the possibility that MRI-guided biopsy might provide histologic clarification of the apparent disparity, we studied use of the new modality at three time points in prostate cancer care: at diagnosis, during active surveillance, and after radical prostatectomy.
Methods: Subjects were 1002 consecutive men who underwent MRI-guided biopsy combining both systematic and lesion-targeted sampling between 2009-2018. Pathologic upgrading was defined as an increase in Gleason Grade group (GG) at structured follow-up biopsy during active surveillance (AS) or at whole-mount sectioning (prostatectomy.) Statistical significance (p<0.05) was assessed using the Mann-Whitney-U test for continuous data, the Chi-square test (or Fisher's exact if necessary) for categorical data, and the Kaplan-Meier estimator to calculate progression-free survival probabilities.
Results: AA men (N=57) had higher rates of prostate cancer at diagnostic biopsy than other men (N=945) (79% AA vs 66% others; p=0.05). GG was similar in both groups: AA vs Other: GG<2, 25% vs 20%; GG3, 12% vs 10%; GG>4, 9% vs 9% (p=0.76). Upgrading at prostatectomy was found in 3/29 (10%) AA men and 32/262 (12%) other men (p=0.45). Among low-risk men in AS, Gleason upgrading during a median follow up of 4 years was found in 5/16 (31%) AA men and 93/274 (34%) other men (p=0.80).
Conclusions: In our cohort studied with contemporary MRI-guided biopsy, aggressiveness of prostate cancer was the same for both groups at initial biopsy, at prostatectomy, and during AS. We found with the improved technology, no significant histologic differences between AA and other men. This suggests that differences previously observed were not based on physiology alone. Furthermore, these data indicate that entry into AS programs for AA men with prostate cancer is appropriate, when low-risk pathology is determined using MRI-guided biopsy.
-
College
PCC
-
Zoom
https://ucla-hipaa.zoom.us/j/92353244220?pwd=dnlQZk8vQ0NNSEtlMFVxV25kRm8rdz09
-
PDF