-
Author
Roberta Palau Antillon -
Co-author
Tracie Lo MD, Theodora Wingert MD, Victor Xia MD, Wendy Ren MD
-
Title
Anesthesia management of liver transplantations in pediatric patients with metabolic disorders: a case series
-
Abstract
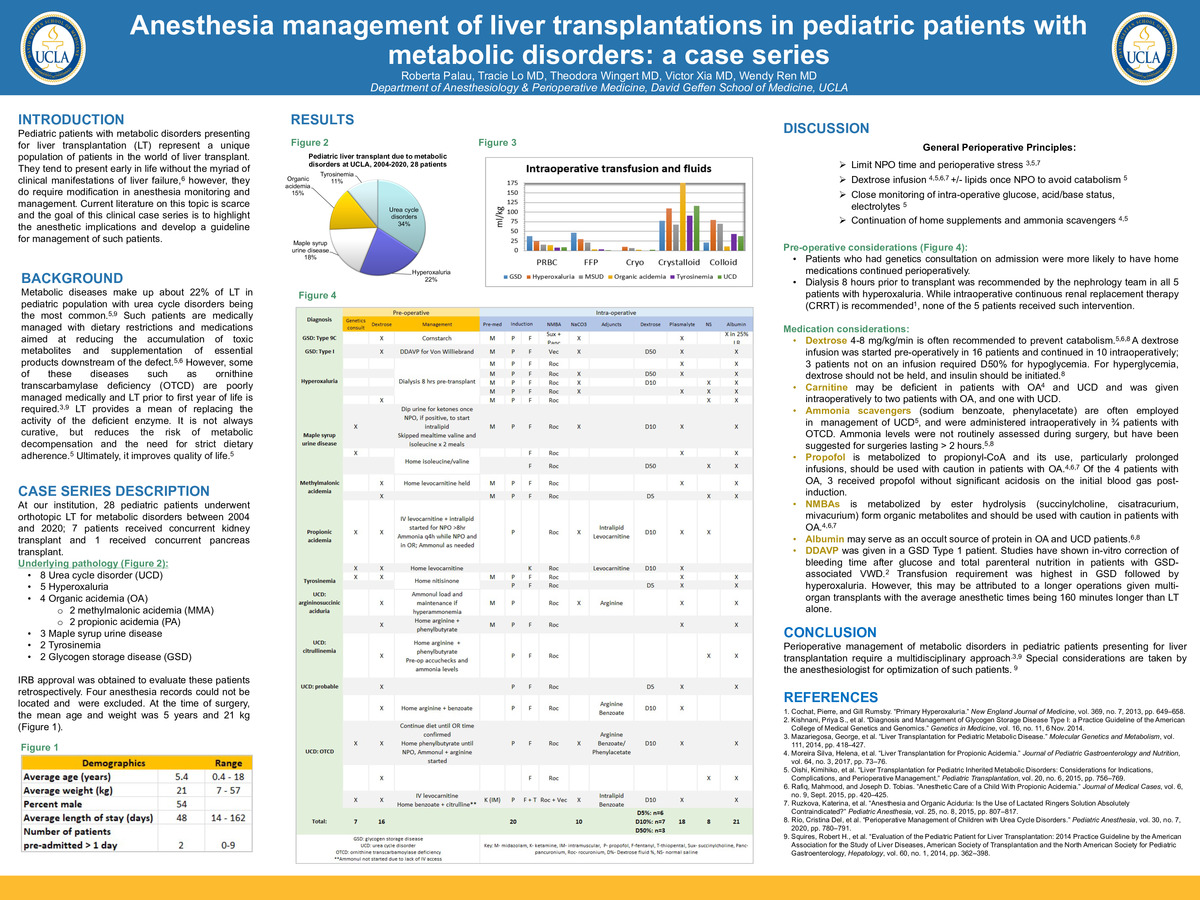
Purpose: Pediatric patients with metabolic disorders presenting for liver transplantation represent a unique population of patients in the world of liver transplant. They tend to present early in life without the myriad of clinical manifestations of liver failure, however, they do require modification in anesthesia monitoring and management. Current literature on this topic is scarce and the goal of this clinical case series is to highlight the anesthetic implications and develop a guideline for management of such patients.
Patients: At our institution, there were 28 liver transplants for metabolic disorders in pediatric patients between 2004 and 2020; 5 patients received concurrent renal transplant and 1 concurrent pancreas transplant. At the time of transplant, the mean age was 5 years, 21 kg, with an average length of stay of 48 days. The underlying pathology included 8 cases of urea cycle disorder (UCD), 6 hyperoxaluria, 5 maple syrup urine disease, 3 tyrosinemia, 2 methylmalonic acidemia, 2 propionic acidemia (PA), and 2 glycogen storage disease.
Results: All patients received general anesthesia with endotracheal intubation. Dextrose is often recommended to prevent catabolism, especially during stress in the perioperative setting. A dextrose infusion was administered in 10/24 patients and 3 patients not on an infusion required D50. Insulin was required in 16/24 patients. Levocarnitine was recommended as part of the genetics evaluation and given intraoperatively in both patients with PA. Hyperammonemia occurs in urea cycle disorders, and ammonia scavengers are often employed as part of the treatment, and were administered intraoperatively in 3/8 of patients with UCD. Propofol emulsion consists of polyunsaturated fatty acids, which are metabolized to propionyl-CoA and could increase the level of propionic acids. Based on the initial blood gas obtained post-induction, 4/24 patients had significant acidosis with pH < 7.3, however, neither of the 2 patients with PA exhibited acidosis after propofol administration.
Conclusion: Perioperative management of metabolic disorders in pediatric patients presenting for liver transplantation require a multidisciplinary approach. Special considerations are taken by the anesthesiologist for optimization of such patients, including prevention of catabolic state, acidosis, and hyperammonemia, induction of anesthesia and fluid management.
-
College
AAC
-
Zoom
-
PDF