-
Author
Cory Johnson -
Co-author
Sharzhad Bazargan-Hejazi, PhD, Peregrina Arciaga, MD
-
Title
Pain and Prejudice: Racial Disparity in Pain Diagnosis and Management in a Large City Healthcare System
-
Abstract
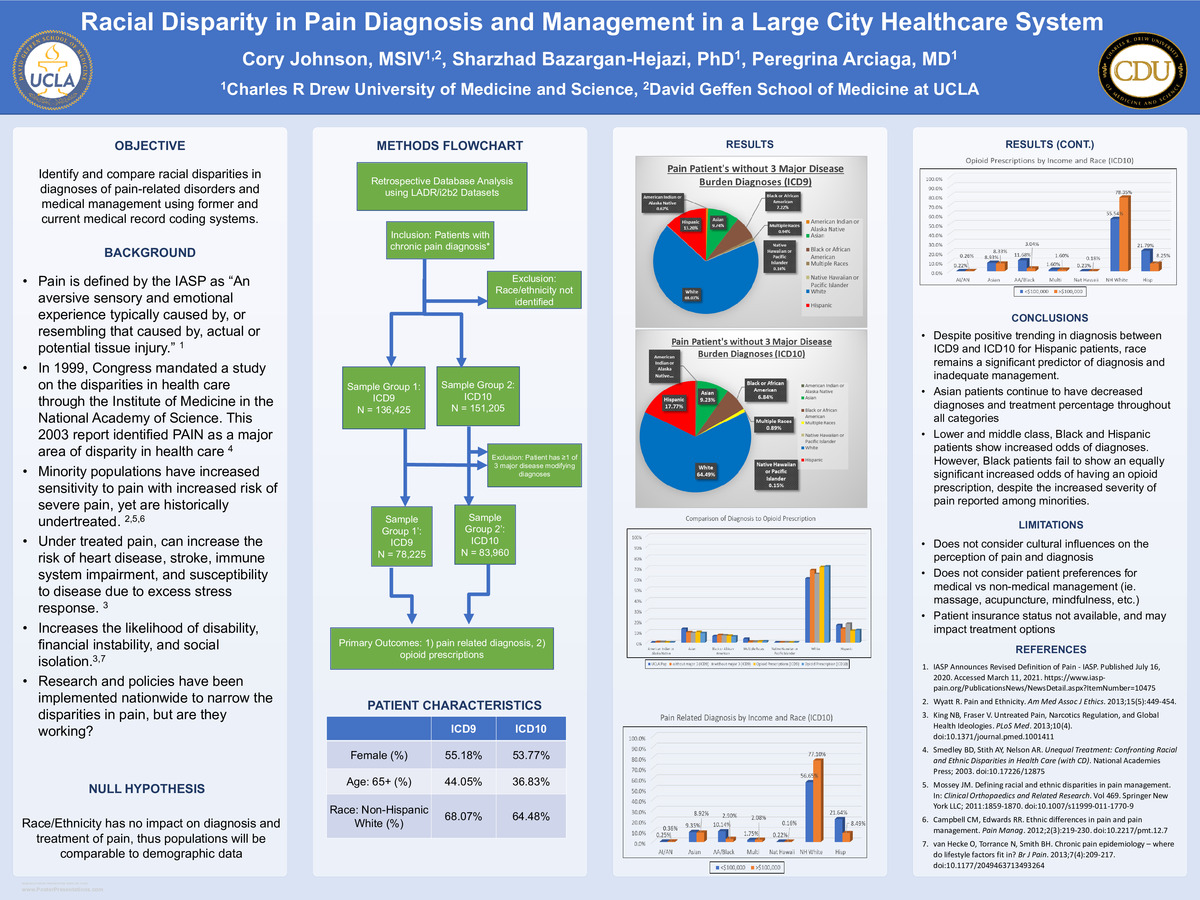
Background: Studies show minorities have enhanced sensitivity to pain with increased severity compared to non-Hispanic white patients. However, in 2003, a congressionally mandated study by the IoM/NAS defined pain as an area of major health disparities. Over the many years since The IoM/NAS study, various reports have given recommendations on how to combat inequities in pain management. Literature falls short of identifying whether these recommendations are being implemented and increasing equity among populations.
Objective(s): Identify and compare racial disparities in diagnoses of pain-related disorders and medical management using former and current medical record coding systems.
Methods:
Retrospective Database analysis of patients within the UCLA Health System diagnosed with the most common chronic pain disorders identified by the UCLA Comprehensive Pain Center charting forms. Patients were categorized by race, ethnicity, and average income of neighborhood using both ICD9 and ICD10 coding systems. Diagnoses and opioid prescriptions were identified among the populations of patients without the major modifiable risk factors and contrasted with UCLA demographic data.
Results:
A two-sample test of comparison and sub-category χ2 test were performed with the data. Overall, it was found that white individuals predominate the pain patient population, for both diagnosis and treatment (64-75%), with significant increases in percentage above their UCLA Health demographic. Asian and Hispanic patients were primarily underrepresented (>3% decrease) in ICD9 data. Hispanic patients showed a 35% increase from ICD9 to ICD10. However, Asian patients were consistently under represented in the patient population throughout both coding systems. Additionally, Black and Hispanic patients making <$100k have significantly greater odds of diagnosis of a pain disorder (3.499 and 2.55, respectively), but Black patients of the same group have only slightly greater odds of receiving an opiate medication (OR=1.24, Hispanic OR=2.64).
Conclusions: Despite the increase in diagnosis among hispanic patients, data suggests that race continues to play a role in chronic pain assessment and management. Non-Hispanic White patients dominate the pain world being diagnosed and treated more often. Asian patients are consistenly underrepresented in the pain population and low/middle class non-Hispanic Black patients are disproportionately undertreated, despite the increased odds of diagnosis. Clinical evaluation continues to have an important role, but pain is a highly personalized experience with an emotional component, that can be modified by cultural lenses. Clinicians should base pain management on a combination of patient experience and culutral lense, rather than race or provider perception.
-
College
UUC
-
Zoom
https://uclahs.zoom.us/j/91441354159?pwd=NThqYUx0dFI4Y1RwLzlOS1k0N0JBQT09
-
PDF