-
Author
Grace Lee -
Co-author
Sonam Kapadia, MD; Albert Lee, MD; Christine Dauphine MD; Junko Ozao-Choy, MD
-
Title
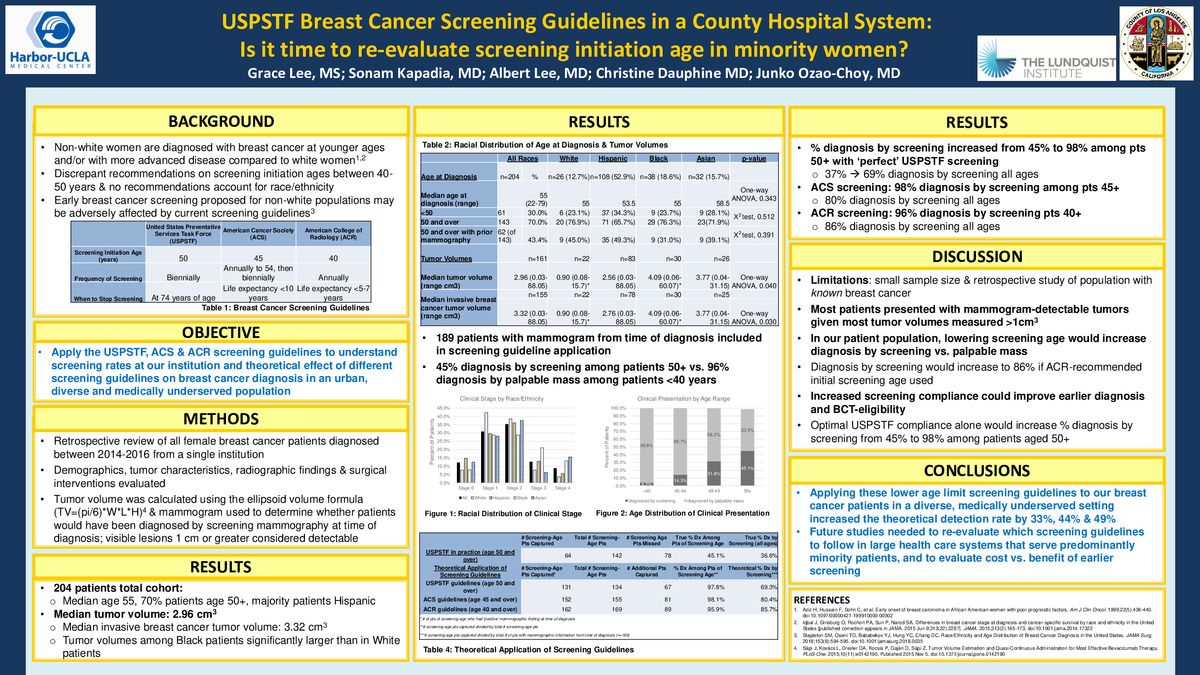
USPSTF Breast Cancer Screening Guidelines in a County Hospital System: Is it time to Re-Evaluate Screening Initiation Age in Minority Women?
-
Abstract
Background and Objectives:
The American College of Radiology (ACR), American Cancer Society (ACS) and United States Preventive Services Task Force (USPSTF) recommend discrepant screening initiation ages varying from age 40 to 50 years. More recently, earlier breast cancer screening for African American women has been proposed due to more advanced-stage disease and younger age at diagnosis. Nonetheless, our large county hospital system follows USPSTF guidelines which recommend initiation of screening at the oldest age of 50. In this retrospective study, we apply the ACR, ACS, and USPSTF screening guidelines to a cohort of our breast cancer patients.
Methods:
All patients with breast cancer diagnosed between 2014-2016 at our institution were retrospectively identified. Demographics (age at diagnosis, race/ethnicity), tumor characteristics (clinical presentation, clinical stage), radiographic findings (tumor dimensions, visibility on mammography), surgical intervention offered/performed were retrospectively collected and univariate analysis was performed. Tumor volume was calculated using the ellipsoid volume formula =(pi/6)*W*L*H based on mammography tumor dimensions. When retrospectively applying screening guidelines, mammograms at time of diagnosis (prior to receiving treatment) were reviewed to determine whether patients would have been diagnosed by screening mammography at time of diagnosis; visible lesions 1 cm or greater were considered positive.
Results:
204 patients were diagnosed with breast cancer from 2014-2016. The actual rate of diagnosis by USPSTF screening guidelines at our institution was only 45% (n=64) among patients age 50 and older (n=143). Tumor dimensions from mammogram at time of diagnosis were available for 189 patients. When USPSTF screening guidelines were theoretically applied to those 189 patients who were 50 and over, an additional 67 patients would have been diagnosed by screening mammography for a total of 98% of patients 50 and over and 69% of the total cohort. When repeated with ACS screening guidelines, 81 additional patients were captured if screening had occurred at the time of diagnosis [98% of patients 45 and older, 80% of all patients]. With the ACR guidelines, 89 additional patients were captured [96% of patients 40 and older, 86% of all patients].
The median age of BCT-eligible patients was higher and tumor volume was significantly smaller than those of BCT-ineligible patients (59 vs. 53 years, p=0.0002; 1.42 cm3 vs. 3.34 cm3, p=0.0289). Median tumor volume was greater among those <50 years of age compared to patients 50 and older (2.93 cm3 vs. 1.87 cm3, p=0.2728). Black patients had significantly larger tumor volumes at diagnosis compared to White patients.
Conclusion:
In addition to presenting at a younger age with more advanced-stage cancer, younger patients at our institution present with larger tumor volumes and may be less eligible for BCT. Given these findings, our patients may benefit from earlier screening. Ultimately, as most patients present with tumors that are mammogram detectable, screening compliance is increasingly vital to improve earlier diagnosis and optimize BCT eligibility. Future studies should include cost-benefit analysis of lowering the screening age among patients and re-evaluation of which screening guidelines to implement in large health care systems that serve predominantly ethnic minority patients.
-
College
AAC
-
Zoom
-
PDF