-
Author
Jeremy-Ann Ham -
Co-author
Wendi LeBrett, MD; Anna Lee, MD; Estebes Hernandez, MD
-
Title
An Un-“Li-”kely Diagnosis The Third Element in a Case of Altered Mental Status
-
Abstract
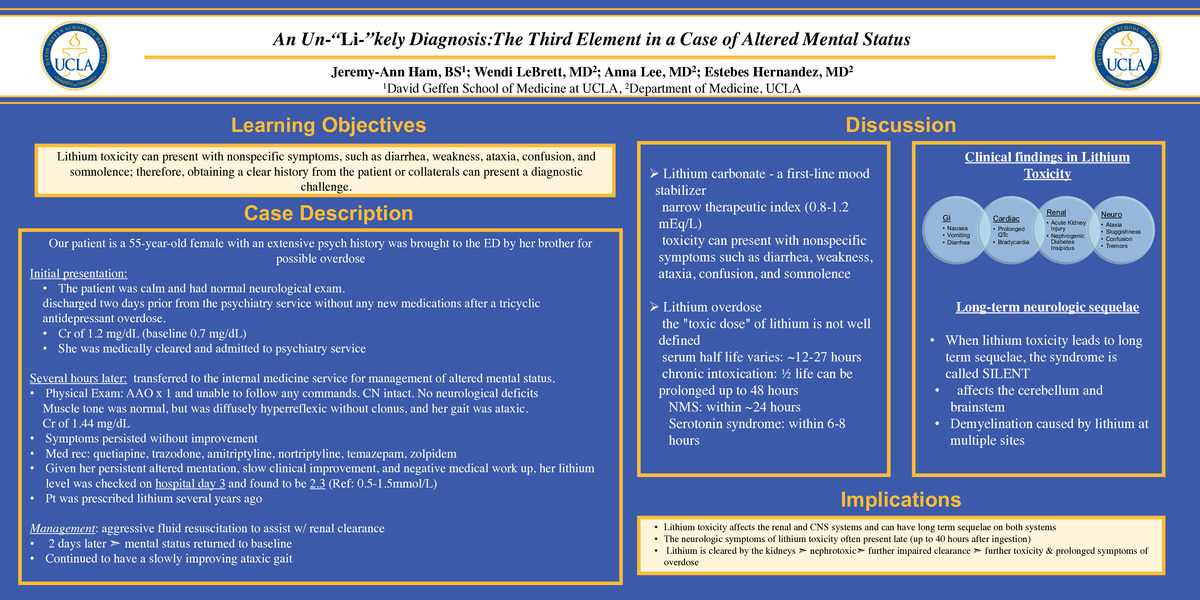
Introduction: Lithium has a narrow therapeutic index and toxicity can present with symptoms such as diarrhea, weakness, ataxia, confusion, and somnolence. The timeline of acute lithium toxicity often differs from other medications and can pose a diagnostic challenge. We present a case of acute lithium overdose with the delayed and prolonged presentation of symptoms from initial ingestion.
Case Description: A 55-year-old female with a history of depression and multiple suicide attempts was brought to the emergency department by her brother for a possible overdose on a substance. On initial presentation, the patient was calm, able to fully participate in the interview, and had a normal neurological exam. She did not admit to ingesting any substances but had been discharged two days prior from the psychiatry service after a tricyclic antidepressant overdose. Labs were notable for a creatinine of 1.2 mg/dL (baseline 0.7 mg/dL). The patient was observed for 12 hours in the emergency department without significant clinical changes at which point she was admitted to the psychiatry service. Several hours later, she had a change in her mental status and was transferred to the internal medicine service. Physical exam was notable for being oriented only to herself and being unable to follow simple commands. Muscle tone was normal. She was diffusely hyperreflexic without clonus, and her gait was ataxic. On transfer, her labs were significant for a white blood cell count of 16.30 x10E3/uL and creatinine of 1.44 mg/dL. Symptoms persisted for over 72 hours from initial presentation. A medication reconciliation was performed and included quetiapine, trazodone, amitriptyline, nortriptyline, temazepam, and zolpidem. Given her persistent altered mentation and slow clinical improvement, a lithium level was checked on hospital day 3 and found to be 2.3 (Ref: 0.5-1.5mmol/L). Further chart review revealed that the patient had been prescribed lithium from her prior therapist several years ago. The patient was managed with intravenous fluids to assist with renal clearance of lithium. Five days after presentation, the patient’s confusion resolved and mental status returned to baseline, although she continued to have a slowly improving ataxic gait.
Discussion: This case illustrates the challenge of diagnosing acute lithium toxicity in the absence of having clinical history from the patient and family. At toxic levels, lithium primarily affects the renal and central nervous systems. The neurologic symptoms of lithium toxicity often present late as the drug requires more time to penetrate the central nervous system. Lithium is cleared by the kidneys but is also nephrotoxic, leading to impaired clearance and prolonged symptoms of overdose. This case highlights the importance of suspecting lithium toxicity if appropriate clinical features are present even in the absence of clinical history as was the case in our patient.
-
College
PCC
-
Zoom
-
PDF