-
Author
Brian Dang -
Co-author
-
Title
Pediatric hematopoietic cell transplantation: Longitudinal trends in body mass index and outcomes
-
Abstract
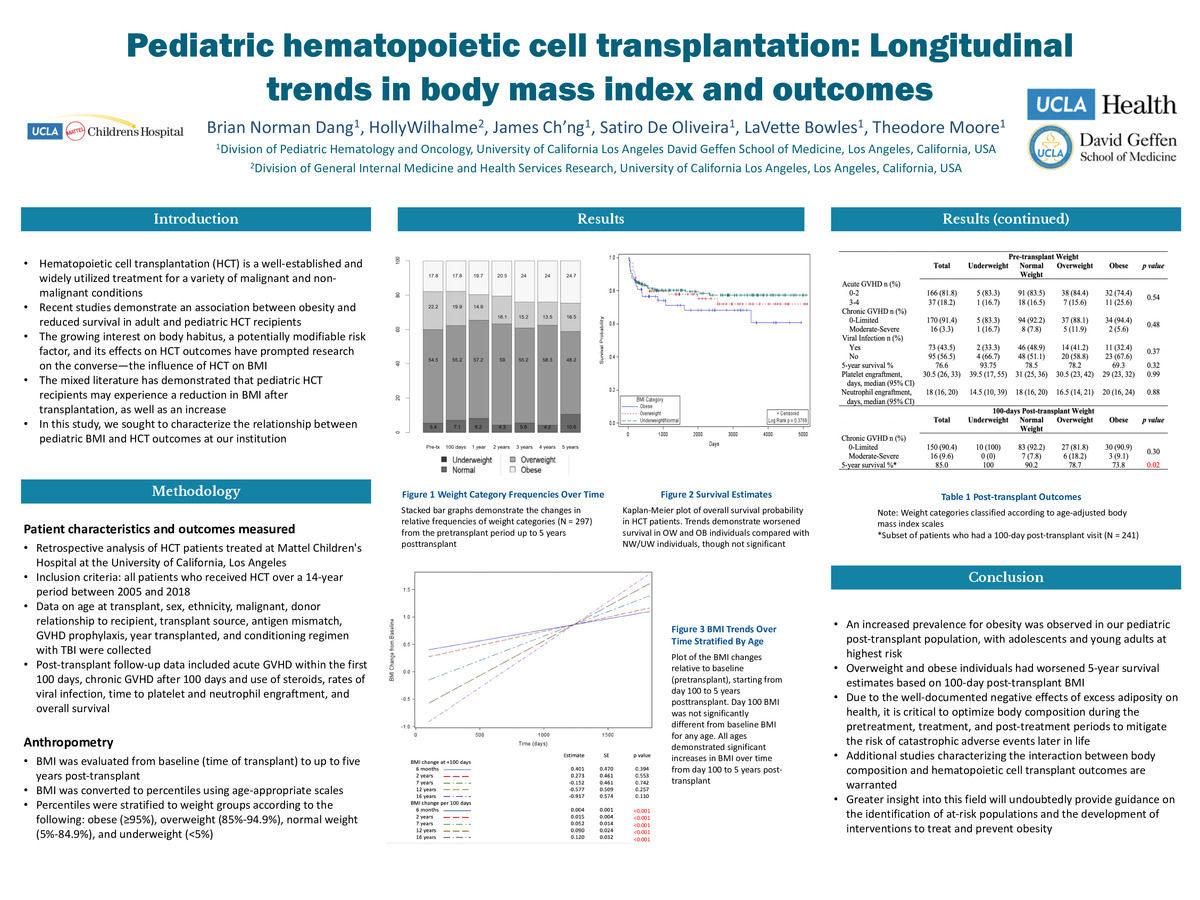
Pediatric recipients of HCT may have a high susceptibility for overweight and obesity, and obesity may negatively impact post-transplant mortality and survival. This is a single-center retrospective analysis of 297 pediatric patients who received HCT between 2005 and 2018. Patients were classified as UW, NW, OW, or OB based on age-adjusted BMI. A mixed-effects linear regression model controlling for patient, disease, and transplant-related characteristics was used to trend weight longitudinally. Comparisons were made between weight category and post-transplant outcomes. In the pretransplant period, 5.4%, 54.5%, 22.2%, and 17.8% of patients were UW, NW, OW, and OB, respectively. Five years post-transplantation, those numbers were 10.6%, 48.2%, 16.5%, and 24.7%. Overall, BMI increased 0.00094 ± 0.0001 kg/m2 each day post-transplant (P < .001), with older individuals demonstrating greater rates of increase. Further, there was a larger BMI increase in patients without TBI compared with those who received TBI (1.29 ± 0.49, P = .008). Rates of acute GVHD, chronic GVHD, and viral infections, in addition to time to platelet and neutrophil engraftment and 5-year survival estimates, were not significantly different based on pretransplant BMI. Overweight and obese individuals had poorer 5-year survival based on 100-day post-transplant BMI (P = .02). Overall, pediatric HCT recipients are at risk of developing obesity, which is associated with decreased survival. Adolescents and young adults demonstrate the highest risk of weight gain, representing a vulnerable population that requires close monitoring, additional interventions, and further research
-
College
AMC
-
Zoom
https://zoom.us/j/99744707260?pwd=Y2RkNFNidWViUHVZQVNYZHMxeHBTZz09
-
PDF