-
Author
Ankur Patel -
Co-author
Troy Sanders, BS, Sujay Alvencar, MD, Alyssa, Choi, MD, Jade Law, MD, Janaki Shah, MD, Karishma Patel, BA, Michelle Nguyen, BS, Taliha Yasin, MD, Daniel Kim, MD, Preeti Prakash, MD, Tahnee Sidhu, MD, Padmavathi Srivoleti, MD, Kirtan Chauhan, MD, Simcha Weissman, MD, Erik Holzwanger, MD, Rohit Dhingra, MD, Aaron Dickstein, MD, Nimisha Parekh, MD, James Tabibian, MD, Osama Altayar, MD, Matthew Ciorba, MD, Jessica Yu, MD, Lea Ann Chen, MD, Liu Yang, MD, Berkeley Limketkai, MD
-
Title
Gastrointestinal Manifestations of COVID-19 Across the United States: A Multi-Center Cohort Study
-
Abstract
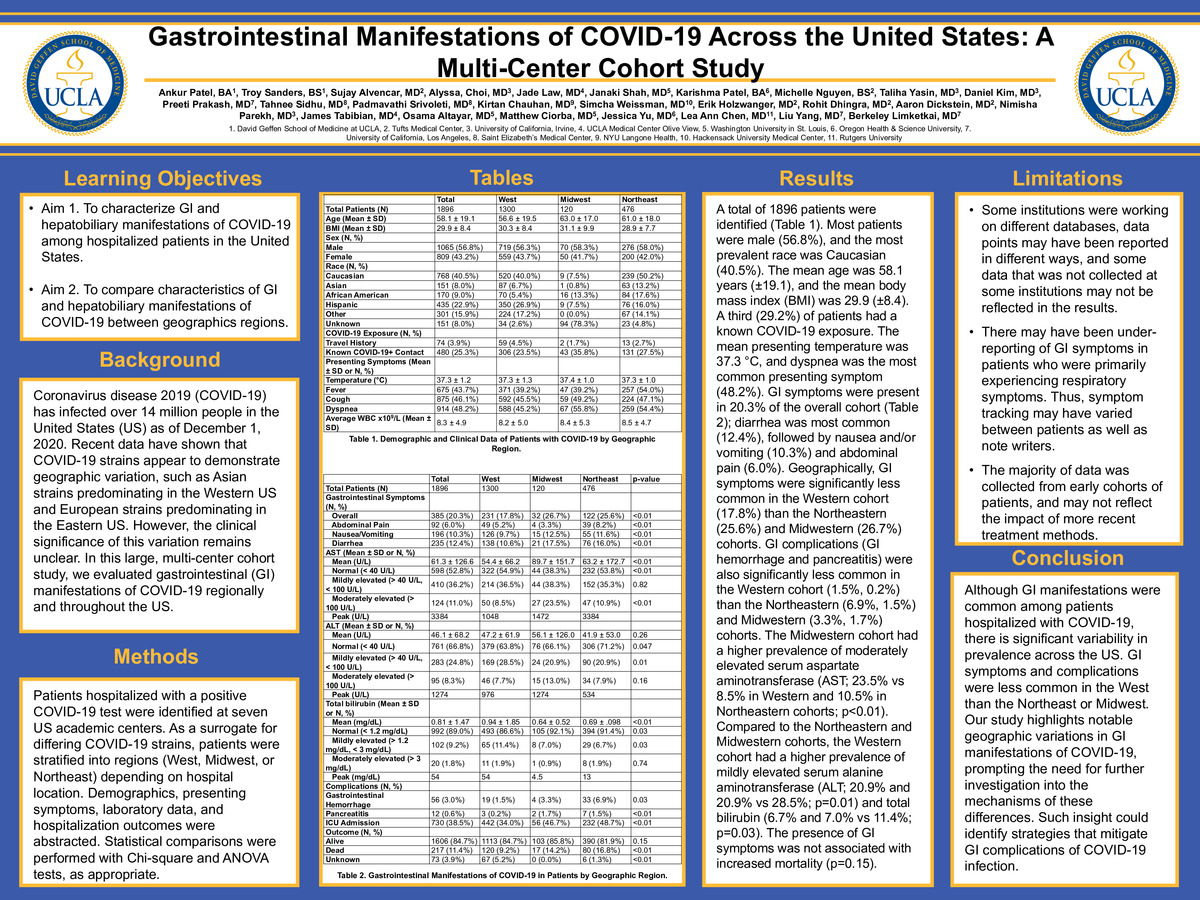
Background: Coronavirus disease 2019 (COVID-19) has infected over 14 million people in the United States (US) as of December 1, 2020. Recent data have shown that COVID-19 strains appear to demonstrate geographic variation, such as Asian strains predominating in the Western US and European strains predominating in the Eastern US. However, the clinical significance of this variation remains unclear. In this large, multi-center cohort study, we evaluated gastrointestinal (GI) manifestations of COVID-19 regionally and throughout the US.
Methods: Patients hospitalized with a positive COVID-19 test were identified at seven US academic centers. As a surrogate for differing COVID-19 strains, patients were stratified into regions (West, Midwest, or Northeast) depending on hospital location. Demographics, presenting symptoms, laboratory data, and hospitalization outcomes were abstracted. Statistical comparisons were performed with Chi-square and ANOVA tests, as appropriate.
Results: A total of 1896 patients were identified (Table 1). Most patients were male (56.8%), and the most prevalent race was Caucasian (40.5%). The mean age was 58.1 years (±19.1), and the mean body mass index (BMI) was 29.9 (±8.4). A third (29.2%) of patients had a known COVID-19 exposure. The mean presenting temperature was 37.3 °C, and dyspnea was the most common presenting symptom (48.2%). GI symptoms were present in 20.3% of the overall cohort (Table 2); diarrhea was most common (12.4%), followed by nausea and/or vomiting (10.3%) and abdominal pain (6.0%). Geographically, GI symptoms were significantly less common in the Western cohort (17.8%) than the Northeastern (25.6%) and Midwestern (26.7%) cohorts. GI complications (GI hemorrhage and pancreatitis) were also significantly less common in the Western cohort (1.5%, 0.2%) than the Northeastern (6.9%, 1.5%) and Midwestern (3.3%, 1.7%) cohorts. The Midwestern cohort had a higher prevalence of moderately elevated serum aspartate aminotransferase (AST; 23.5% vs 8.5% in Western and 10.5% in Northeastern cohorts; p<0.01). Compared to the Northeastern and Midwestern cohorts, the Western cohort had a higher prevalence of mildly elevated serum alanine aminotransferase (ALT; 20.9% and 20.9% vs 28.5%; p=0.01) and total bilirubin (6.7% and 7.0% vs 11.4%; p=0.03). The presence of GI symptoms was not associated with increased mortality (p=0.15).
Conclusions: Although GI manifestations were common among patients hospitalized with COVID-19, there is significant variability in prevalence across the US. GI symptoms and complications were less common in the West than the Northeast or Midwest. Our study highlights notable geographic variations in GI manifestations of COVID-19, prompting the need for further investigation into the mechanisms of these differences. Such insight could identify strategies that mitigate GI complications of COVID-19 infection.
-
College
AMC
-
Zoom
-
PDF