-
Author
Christine Liu -
PI
Karin Nielsen-Saines
-
Co-Author
Christine Liu
-
Title
Assessment of maternal and infant antibody response to COVID-19 and transplacental transfer ratios at labor & delivery
-
Program
Global Short-Term Training Program
-
Other Program (if not listed above)
-
Abstract
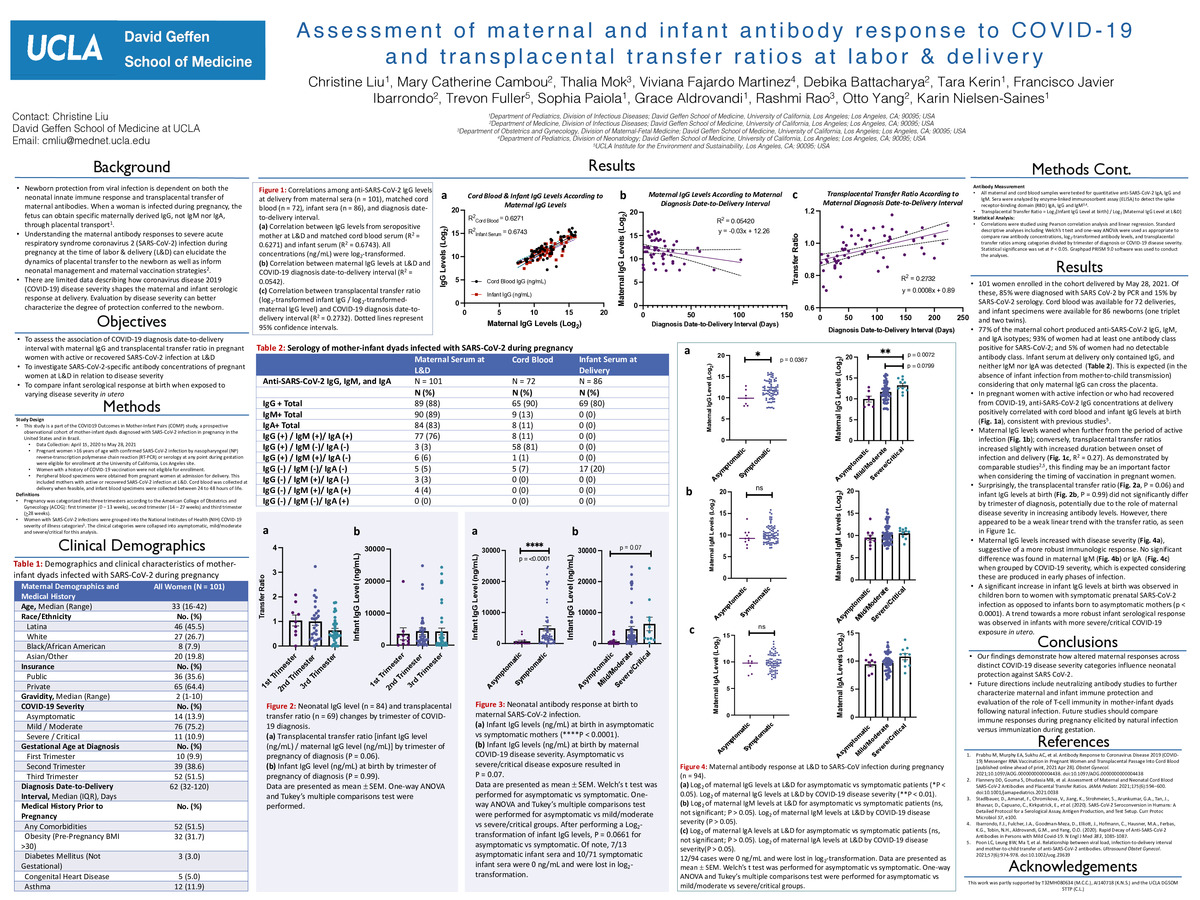
Background: Newborn protection from viral infection is dependent on both the neonatal innate immune response and transplacental transfer of maternal antibodies. Understanding the maternal antibody responses to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection during pregnancy at the time of labor & delivery (L&D) can elucidate the dynamics of placental transfer to the newborn as well as inform neonatal management and maternal vaccination strategies. There are limited data describing how coronavirus disease 2019 (COVID-19) disease severity shapes the maternal and infant serologic response at delivery. Evaluation by disease severity can better characterize the degree of protection conferred to the newborn.
Objectives: To investigate SARS-CoV-2-specific antibody concentrations of pregnant women at L&D in relation to disease severity, and to compare infant serological response at birth when exposed to varying disease severity in utero
Study Design: This study is a part of the COVID19 Outcomes in Mother-Infant Pairs (COMP) study, a prospective observational cohort of mother-infant dyads diagnosed with SARS-CoV-2 infection in pregnancy in the United States and in Brazil. A total of 101 pregnant women at the Los Angeles site were delivered between April 15, 2020 to May 28, 2021. Maternal and cord blood sera as well as infant blood specimens were collected.
Results: The study cohort consisted of 101 parturient women, among which 72 matched cord blood and 86 infant specimens were available. 77% of the maternal cohort produced anti-SARS-CoV-2 IgG, IgM, and IgA isotypes; 93% of women had at least one antibody class positive for SARS-CoV-2; and 5% of women had no detectable antibody class. Infant serum at delivery only contained IgG, and neither IgM nor IgA was detected. Maternal IgG levels waned when further from the period of active infection; conversely, transplacental transfer ratios increased slightly with increased duration between onset of infection and delivery (R2 = 0.27). Maternal IgG levels increased with disease severity, suggestive of a more robust immunologic response. No significant difference was found in maternal IgM or IgA when grouped by COVID-19 severity. A significant increase in infant IgG levels at birth was observed in children born to women with symptomatic prenatal SARS-CoV-2 infection as opposed to infants born to asymptomatic mothers (p < 0.0001). A trend towards a more robust infant serological response was observed in infants with more severe/critical COVID-19 exposure in utero.
Conclusions: Our findings demonstrate how altered maternal responses across distinct COVID-19 disease severity categories influence neonatal protection against SARS CoV-2.
-
PDF
-
Zoom
https://uclahs.zoom.us/j/95249194129?pwd=VDdwVFB6bU9lNEI5TVVjc2RQLzhOZz09