-
Author
Dyvon Walker -
Co-author
Renea Sturm, Doug Daniels, Jesse Mills, Sriram Eleswarapu
-
Title
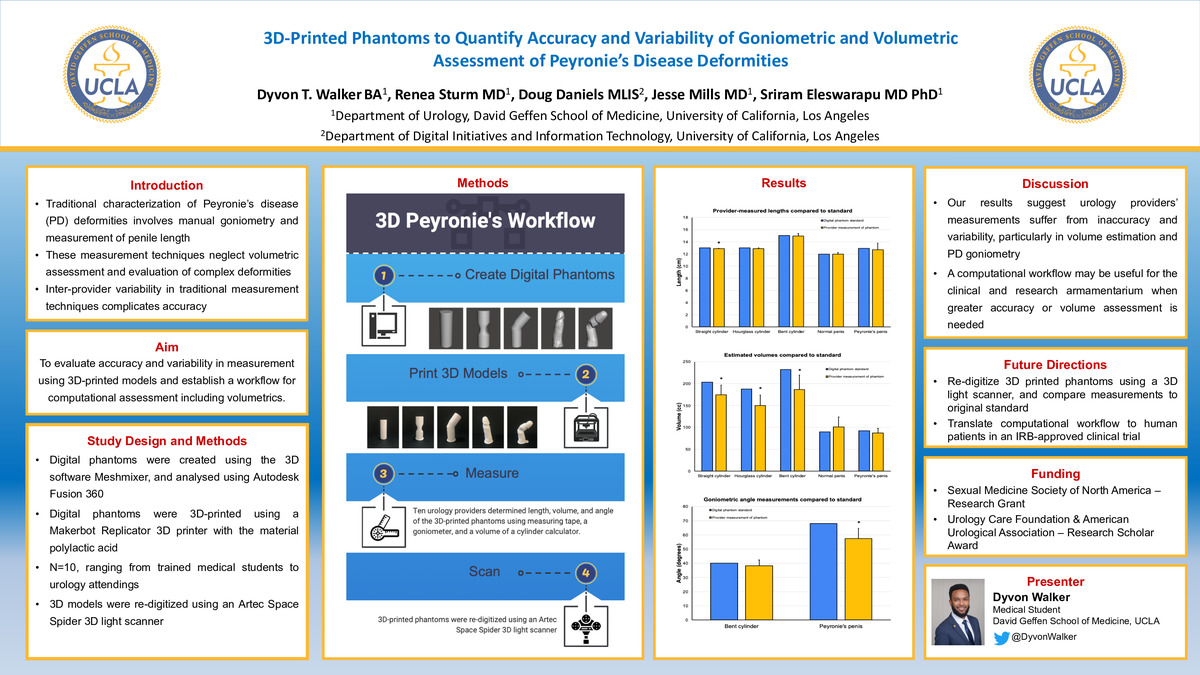
3D-printed phantoms to quantify accuracy and variability of goniometric and volumetric assessment of Peyronie's disease deformities
-
Abstract
INTRODUCTION AND OBJECTIVE: Characterization of Peyronie’s disease (PD) deformities involves manual goniometry and measurement of penile length. These techniques neglect volume loss or hourglass, a source of bother. Inter-provider variability complicates accuracy. Using standardized 3D-printed models, we aimed to evaluate accuracy and variability in measurement and establish a workflow for computational assessment including volumetrics.
METHODS: Five 3D phantoms were created digitally: 13.0 cm cylinder, 13.0 cm hourglass cylinder, 15.0 cm cylinder with 40˚ angulation, 12.0 cm straight penis, and 12.9 cm PD penis with 68˚ angulation and hourglass. Lengths, volumes, and curvature angles were determined computationally to serve as standards. Each phantom was printed using a Makerbot Replicator+. Ten urology providers determined length, angle, and volume of phantoms using measuring tape, goniometer, and volume calculator. Means ± SD were calculated. To determine accuracy, depending on data distribution, a t-test or Wilcoxon rank sum test was used to compare provider-determined vs. computationally acquired measurements.
RESULTS: Lengths for cylinder, hourglass cylinder, angled cylinder, straight penis, and PD penis were 12.9 ± 0.9 cm (p=0.0003), 12.9 ± 1.61 cm (p=0.058), 15.0 ± 4.3 cm (p=0.52), 12.0 ± 2.3 (p=0.68), and 12.7 ± 10.8 (p=0.36), respectively. Volumes were 174 ± 22 cc (p=0.003), 150 ± 24 cc (p=0.0008), 186 ± 33 cc (p=0.004), 101 ± 23 cc (p=0.16), and 87 ± 11 cc (p=0.23), respectively. Curvature angles from bent cylinder and PD phantoms were 38.3˚ ± 3.9˚ (p=0.25) and 57.5˚ ± 7.2˚ (p=0.006), respectively. Discrepancy between goniometry and computationally determined angle ranged 3˚ to 13˚.
CONCLUSIONS: Our results suggest urology providers’ measurements suffer from inaccuracy and variability, particularly in volume estimation and PD goniometry. A computational workflow may be useful for the clinical and research armamentarium when greater accuracy or volume assessment is needed. Further work using 3D image-capture techniques (Siapno et al., SPU 2019) may allow translation to patient evaluation.
Source of Funding: Research Grant from Sexual Medicine Society of North America; Research Scholar Award from the Urology Care Foundation & American Urological Association.
-
College
AAC
-
Zoom
-
PDF